Clinic for Implant
&
Orthodontic Dentistry, procedures explained, offers, information,
How Bite Splints and Dental Occlusion Adjustments Can Help with Relief from Ear Tinnitus and TMJ Pain?
Living with ear tinnitus and TMJ pain can be incredibly challenging, affecting both our physical and emotional well-being. However, as a dentist, I am here to shed light on a lesser-known solution that can provide relief for these conditions. By addressing occlusal interferences and utilising custom-made bite splints, we can effectively reduce ear ringing and alleviate TMJ pain, ultimately improving your quality of life.
Living with ear tinnitus and TMJ discomfort can be extremely difficult and detrimental to our physical and mental health. But as a dentist, I'm here to highlight a less well-known treatment that helps alleviate these symptoms. We can successfully minimise ear ringing and relieve TMJ pain by correcting occlusal interferences and using personalised bite splints, thereby enhancing your quality of life.
Recognising the Relationship:
It is impossible to emphasise the complex relationship between tooth occlusion and ear tinnitus or TMJ pain. Occlusal interferences, which lead to imbalances in the jaw joint, might be the result of misaligned teeth, a bad bite, or persistent grinding and clenching. These imbalances can result in ear tinnitus and TMJ pain, which can cause discomfort, decreased functionality, and a general decline in wellbeing.
Occlusal Adjustments for Relief:
Making occlusal modifications is one of the most important strategies for dealing with these problems. A qualified dentist can find interferences and imbalances by thoroughly analysing your teeth's alignment and evaluating your bite. We can eliminate tension on the jaw joint and the resulting symptoms of ear tinnitus and TMJ pain by making exact changes to your dental occlusion.
Customised Bite Splints:
When occlusal modifications alone may not be enough to relieve pain, using bite splints can be quite helpful. Bite splints, commonly referred to as removable appliances, are made-to-measure tools used to realign the jaw and offer a secure, comfortable position for biting. These splints not only relieve pressure on the jaw joint but also guard the teeth from wear and tear caused by clenching and grinding. Patients who use bite splints on a regular basis report less ringing in their ears and TMJ pain, as well as enhanced jaw mobility and better oral health.
Getting Professional Assistance:
Consult with a dental expert who specialises in occlusion and temporomandibular joint issues if you are experiencing ear tinnitus, TMJ pain, or TMJ clicking. Our knowledgeable staff at Clinic For Implant & Orthodontic Dentistry, located at 7 Chapel Road in Worthing, BN11 1EG, is committed to offering these patients individualised attention and successful treatments. To take the first step towards receiving the assistance you need, schedule a consultation right away.
Despite the difficulty of dealing with ear tinnitus and TMJ pain, relief is possible with the correct dental treatment. An expert dentist can significantly lessen ear ringing and TMJ symptoms by resolving occlusal interferences and deploying bespoke bite splints. Reach out to our dentist office right now to start your journey towards a better, pain-free life and don't let these conditions hold you back.
What is Root canal treatment?
If you are experiencing severe tooth pain, extreme sensitivity, tooth discoloration, swollen gums, a recurring abscess on the gum line or a fissure in a filling, or if you have sustained a traumatic injury to your teeth, you may require a root canal to save your tooth.
The prospect of undergoing a root canal for the first time can be intimidating. In situations where a standard filling cannot save the tooth, a root canal can provide a relatively quick and painless solution.
DO I REQUIRE A ROOT CANAL PROCEDURE OR ENDODONTIC TREATMENT?
If you are experiencing severe tooth pain, extreme sensitivity, tooth discoloration, swollen gums, a recurring abscess on the gum line or a fissure in a filling, or if you have sustained a traumatic injury to your teeth, you may require a root canal to save your tooth. If your dentist believes you are likely to need a root canal, they will take an X-ray and may test for temperature sensitivity; they may also perform comprehensive imaging. If you have an abscess, your dentist may prescribe antibiotics to treat the infection before commencing treatment, or he or she may recommend a root canal.
IF I REQUIRE A ROOT CANAL, WHAT IS THE NEXT STEP?
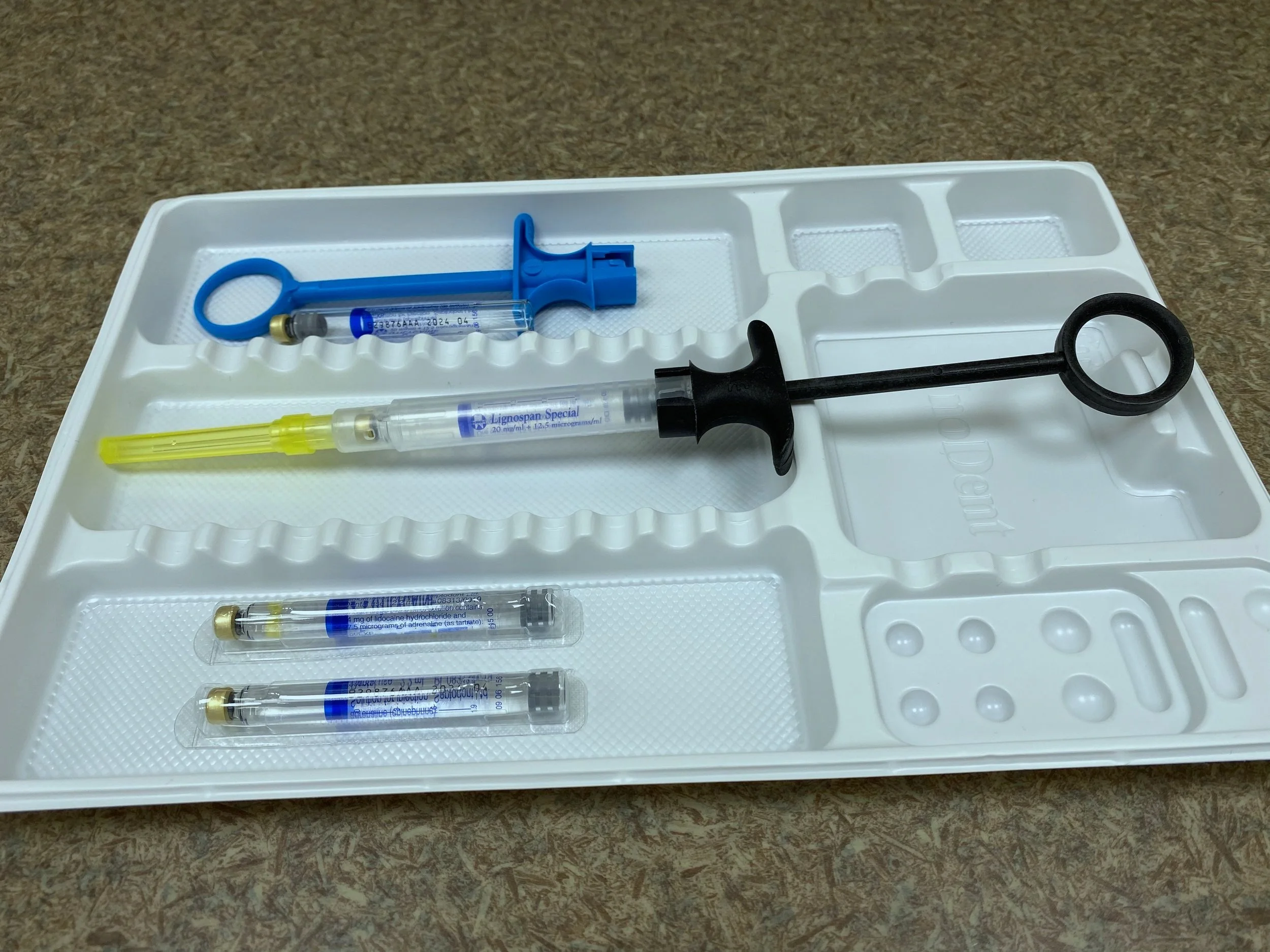
It is essential that you comprehend the root canal procedure, the risks and benefits of the treatment, as well as the treatment's complexity. Root canal treatments are now specially registered with the GDC, and in some cases, your dentist may advise you that a referral to a dentist with a special interest in root canals or endodontics is necessary to ensure long-term success and provide the most effective treatment. Local anaesthesia will be administered to ensure that your root canal treatment is painless. A rubber dam will be inserted around the tooth to maintain a dry environment. An access hole will be drilled, and then decayed nerves and detritus will be removed with files. Then, the root canal will be filled with a polymer compound. Then, a temporary filling may be placed, or the ultimate filling may be completed during the same appointment in some instances.
MY ROOT CANAL TREATMENT WILL IT BE PAINFUL?
Root canal treatment has an unjust reputation for being painful, primarily because patients typically discover they need one after experiencing excruciating tooth or gum pain. As local anaesthetic will be used throughout your treatment, you will experience minimal discomfort at most. 24-72 hours of soreness and discomfort are common following endodontic treatment.
HOW MUCH DOES THE TREATMENT OF A ROOT CANAL COST?
For a cost of a root canal please visit our website fee page HERE. In many cases, a root canal can prevent the need for an extraction, and if you take good care of your teeth and tissues after the procedure, root canal treatment can last a lifetime with routine maintenance and checkups.Please note that following a root canal, you will need a restoration such as a filling or crown. In addition to the cost of root canal, the cost of a filling or crown will be added.
WHAT IS THE RATE OF SUCCESS FOR ROOT CANALS?
90% approximately. In extremely uncommon instances, we may discover additional infection in the root after performing a root canal and may need to administer additional treatment. In extremely rare circumstances, a root canal may not be able to save the tooth. However, as a treatment with a success rate of 90% and durability for the majority of patients, a root canal is typically an excellent method to avoid extraction. Our opinion is that root canals should be performed by a practitioner with postgraduate experience in this discipline. Treatments and technologies have progressed, increasing the success rate of root canals.
WHAT SHOULD I DO AFTER THE TREATMENT OF MY ROOT CANAL?
After your treatment, you may desire to take an over-the-counter pain reliever, such as Aspirin or Ibuprofen, for minor pain or sensitivity. Ensure that you finish any antibiotics prescribed by your dentist and that you continue to brush and floss as usual. Long-term vigilance with brushing and flossing is essential for maximising the effectiveness of root canal therapy. If properly maintained, a root canal can last a lifetime. In the past, patients were typically told that a root canal would last between 8 and 10 years, but we'd add that the longer you want your root canal to last, the better you must care for your teeth and gums! Not smoking, flossing and scrubbing your teeth religiously, and visiting your dentist and hygienist on a regular basis will all contribute to the longevity of your root canal. According to research, most post-root canal procedures should include a crown inlay and post.
IS A ROOT CANAL A VERY DELAYED PROCEDURE?
Root canal procedures can take between two and three hours, depending on their complexity. We may be able to complete your root canal in a single appointment, which will take approximately 60 minutes, but root canals are technically challenging, so time must be taken to achieve the best results.
What are the most prevalent root canal treatment myths?
Root canals are an excruciating procedure. Yes, if you require a root canal, you may arrive at the clinic in agony, but this should subside once we begin treatment! Patients frequently report that the relief they experience once root canal therapy begins and we can stop the tooth and gum pain they've been experiencing is immense, and that root canal therapy itself should be painless.
The cost of root canals is high. They are more expensive than standard composite fillings, but significantly less expensive than dental implants, and if you detect your dental issues early, a root canal may prevent you from needing an implant in the future. A naturally saved root canal is always preferable to an implant, and while the prospect of spending up to three hours in the dentist's chair may be daunting, it's worth it to be pain-free and save your tooth!
That root canals are time-consuming. We may be able to complete your root canal treatment in a single visit, but even if it requires multiple visits, it's a surprisingly quick and effective method to save your tooth!
Root canals have a lengthy recovery period. Similar to after having a filling, you may experience some sensitivity, but this should subside within two days. Additionally, we recommend biting a little more gently on the treated tooth for the next day or so, and Ibuprofen can be consumed. Aside from this, there is virtually no recovery period following a root canal. Just be sure to brush and floss thoroughly, and business as usual will resume after your procedure.
That root canals are not durable. We will provide you with the highest conceivable standard of care. Then the floor is yours. If you take good care of your teeth after root canal therapy, root canals can last for many years. In general, root canals that are not performed accurately fail. Remember to inquire honestly about your dentist's experience with root canal treatments. Ask them if they use a microscope and for their assessment of the risks and benefits of the treatment. Root canal treatment may appear to be costly, time-consuming, and intimidating, but if performed by the right practitioner with the necessary experience, it should be a pleasant and successful procedure at Clinic for Implant & Orthodontic Dentistry, 7 Chapel Road, Worthing (West Sussex), telephone number 01903-821822.
A Guide to Wear-Down Teeth: Signs, Symptoms, and Dental Treatments
In this article, we will delve into the causes, symptoms, and available dental treatments for worn-down teeth. Understanding the aetiology of this condition, recognizing its symptoms, and exploring the various treatment options can help you maintain optimal oral health.
Recognising Wear-Down Teeth: Signs, Symptoms, and Dental Treatments
Introduction:
It is my pleasure as a dentist to provide some general information inform about worn-down teeth, their causes, symptoms, and the possible therapies for this prevalent dental condition. Worn-down teeth, sometimes referred to as tooth wear or dental erosion, happen when the enamel, the teeth's protective outer coating, gradually erodes as a result of many causes. Knowing the cause, identifying the symptoms, and getting the right dental care can help stop additional harm and improve your oral health.
Worn-Down Teeth Causes: A number of factors can lead to worn-down teeth, including:
Bruxism:
Teeth grinding or clenching, frequently unintentionally while sleeping, places an excessive amount of pressure on the teeth and causes enamel erosion and attrition.
Acidic Foods and Drinks:
Regularly consuming acidic foods and drinks (such citrus juices and soft drinks) will eventually destroy the enamel.
Brushing Too harsh:
Using a toothbrush with harsh bristles or brushing too vigorously can both lead to enamel damage.
Acid Reflux:
Acid reflux can expose teeth to stomach acid, which erodes the enamel. This condition is known as gastroesophageal reflux disease (GERD).
Certain Drugs:
Drugs that contain aspirin or antihistamines, for example, might produce dry mouth, which reduces saliva flow and makes teeth more prone to wear.
Age:
Over time, natural wear and tear can progressively wear away the enamel, increasing the risk of erosion.
Other Factors:
Chewing on hard things (such ice or pen caps), misaligned teeth, and other underlying medical disorders can also lead to tooth deterioration.
Signs of worn-down teeth include:
The following signs of worn-down teeth include:
Increased Sensitivity of the Teeth:
Worn enamel exposes the underlying dentin, increasing sensitivity to meals that are spicy, cold, sweet, or acidic. Teeth that Look Flattened or Rounded: Enamel loss can give teeth that bite surfaces a rounded or flat look.
Changes in Tooth Colour:
Teeth may seem yellow or discoloured as enamel erodes. Small chips, fissures, or rough edges may appear on worn-down teeth.
Pain in the teeth:
Serious tooth wear may cause pain or discomfort, particularly while chewing or biting.
Dental Procedures for Damaged Teeth:
Depending on the severity of the issue, a number of treatment methods are available for worn-down teeth:
Dental Bonding:
In minor circumstances, dental bonding can be performed to restore the shape, function, and appearance of the afflicted teeth by coating them with tooth-colored resin.
Dental crowns:
Dental crowns may be suggested in cases of more severe tooth wear. These specialised tooth-shaped caps completely encase the tooth, giving it strength, protection, and a more appealing appearance. When the damage is too severe for a conventional filling but does not require a full crown, inlays and onlays—also known as indirect fillings—are employed. They are created in a dental lab, and after that, the tooth is attached to them.
Orthodontic therapy:
If misaligned teeth are a factor in the deterioration of certain regions, orthodontic therapy with braces or invisible aligners may be suggested to rectify the alignment and stop further deterioration.
Nightguards or Splints:
If bruxism is wearing down your teeth, a nightguard or splint can be designed specifically for you to protect your teeth while you sleep and lessen the forces that cause grinding or clenching. Lifestyle Modifications: It's critical to pinpoint and address the root causes of tooth deterioration. Enamel erosion can be stopped by altering diet and dental hygiene practises, cutting back on acidic food and drink intake, brushing correctly, and addressing medical disorders like acid reflux.
Conclusion:
The key to dealing with worn-down teeth is to understand the causes, identify the symptoms, and seek the proper dental care. I advise you to make an appointment with a dentist if you notice any indications of tooth wear. A thorough examination will reveal the full amount of the harm, allowing for the creation of a customised treatment strategy that will restore your smile and safeguard your dental health. Keep in mind that early treatment is essential for avoiding additional issues and preserving a beautiful, healthy smile.
Diet Advise following Full Jaw Implant Surgery.
All-on-4 implant surgery is a treatment option for those with periodontal disease or tooth decay. The procedure involves placing implants in the jaw to support a full arch of replacement teeth. After the surgery, patients can expect some adverse effects, including minimal oozing, swelling, tense jaw and facial muscles, and site-specific pain. These symptoms are temporary and can be managed with over-the-counter pain medication. It is important to rest for the first three to four days, then gradually resume normal activities and exercise.
All-on-4 implant surgery is a thorough and successful treatment for periodontal disease and tooth decay, in cases where an entire upper or lower arches are missing or irreparable. Before the benefits of All-on-4 implant surgery take full impact, you can anticipate certain adverse effects after surgery. Possible symptoms include:
- Minimal oozing
- Swelling
- Tense jaw and facial muscles
- Sore throat and/or trouble swallowing
- Site-specific pain
If you experience adverse effects, they are transient and often subside after one week. Any pain or discomfort can be alleviated with over-the-counter drugs such as Paracetamol, Aspirin, or Ibuprofen.
It is very imortant to rest for the first three to four days. After that period of time, and as tolerated, you may resume normal activities and exercise.
However, dietary limitations last longer. These constraints can be divided into two time categories:
- First three weeks after surgery
- From three to six weeks after surgery
Knowing which foods are acceptable to eat following the surgery are crucial, as they will help you with the following;
- Reduces the impact of any pain and/or swelling
- Promotes a rapid recovery
- Maximise the benefits of your All-on-4 operation
If you already have dietary restrictions due to a medical condition (such as diabetes), you should visit a physician or trained nutritionist for advice.
Blender for soft food diet - after surgery, a blender will be your best buddy.
3 Weeks Post-Surgery: Eating on a Liquid Diet
Your mouth, jaw, and throat are likely to be painful for either a few days or up to three weeks after surgery, however any pain or swelling will progressively lessen. As a result, eating might be unpleasant or challenging. During this time a liquid diet without chewing is required.
Here are some considerations to make during this time period;
- The majority of pain post surgery is felt immediately after the surgery. It may be challenging to open your mouth and swallow. If your jaw feels rigid, making it difficult to open your mouth, try massaging it with an ice pack.
- Liquids can be consumed shortly after surgery. In the first 48 hours, you should only consume cool liquids. If you intend to consume something hot, do so until after the anaesthetic has worn off and all bleeding has ceased. It is best to avoid hot or spicy liquids until the third or fourth postoperative day.
- Hydration is key! It's important to consume a great deal of fluids, but in tiny quantities and often throughout the day. Once the anaesthetic has worn off and you feel comfortable enough, you should consume clear fluids shortly after surgery. Fluids will restore and maintain the tissue's moisture for optimal healing, regardless of whether there is drainage following the procedure.
- You will experience hunger as a result of consuming just liquids and avoiding solid foods for the first three weeks following All-on-4 implant surgery. In addition, optimal nutrition is necessary to avoid illness and accelerate recovery. Ensure that the fluids you consume during the day are nutrient-rich and that you consume them often. Given that you have just undergone oral surgery, it is expected that your intake would be lower than usual. However, you must bear in mind that nourishment is essential to healing, and without it you may experience a delay. Following is a list of foods that can be consumed during the first one to two weeks following surgery.
Important - do NOT use a straw when consuming liquids or liquidised food. The sucking movement might loosen blood clots, causing more bleeding and delaying the healing process.
What foods may I consume during this time?
There are numerous liquid foods that can be consumed during the first three weeks following All-on-4 implant surgery. The following are examples of consumable liquids;
- Soup broths (bouillon - beef, poultry, and vegetable)
- Creamy soups (without solids)
- Coconut liquid
- Kefir drinks
- Fruit juices
- Tea/coffee
- Warm cocoa
- Milk, including all forms of cow milk, from fat-free to whole
- Milk derived from nuts or peas
- Milkshakes
- Yogurt drinks
- Meal substitute shakes
- Protein shakes
- Smoothies
- Sodas
- Gelatine (e.g. Jelly)
- Custard
- Ice cream
- Frozen fluids, like fruit ices or popsicles
- Frozen yoghurt
When consuming milkshakes, yogurt drinks, fresh fruit jucies, smoothies and protein shakes, the consistency should be light enough for easy sipping. As the days pass and you feel you can stomach it, you can consume heavier shakes.
When you need to increase your calorie intake, put the following foods in your shakes:
Whites of powdered eggs, milk powder products, instant breakfast mixes (e.g., instant oatmeal), butter, margarine, or oil, sugar, syrup, or honey, or brewing yeast.
Sample Menu for first three Weeks After Surgery
Following is an example of a one-day menu for a fluid diet immediately following All-on-4 surgery. It is vital to note that you should have snacks to ensure that you receive the necessary nutrients and calories for recuperation.
Breakfast
- Fruit juice or smoothie
- Cup of tea or coffee
- Yogurt
- Glass of water
Breakfast Snack
- Glass of fruit juice
- Glass of water
Lunch
- Meal replacement drink
- Cup of broth
- Jelly
- Glass of water
Dinner
- Cup of broth or soup that has been strained
- Cup of fruit juice
- Yogurt
- Glass of water
Evening Snack
- Ice cream or frozen yogurt
- Warm cocoa
- Glass of water
3 weeks to up to 6 weeks after surgery; A soft food diet
After the pain subsides, you will feel more capable of transitioning from a liquid diet to a soft food diet. During the weeks and months following surgery, it is vital to remember that your jaw is still mending and the implants are attempting to integrate.
The process by which the jaw creates a biological bond with the implant screws is known as osseointegration. To ensure that this occurs correctly, you must continue to monitor your diet.
During the inital three months, you MUST avoid consuming meals that are - heard, chewy or crunchy and that require less chewing.
What foods may I consume during this time?
After three weeks, the following are examples of things you can add to your diet;
- Anything that is mashed or puréed, such as - mash potato, fruits, vegetables
- Everything soft, such as - bananas and melons
- Everything in a can and lacking skin and seeds
- Anything baked or cooked to a tender texture
- Soft breads, cakes
- Cooked pasta (soft)
- Noodles
- Quinoa, cous cous
- Eggs - poached, scrambled
- Pureed sauces
Example Menus for three weeks to six weeks:
This is a sample menu for a one-day soft food diet after surgery. It is vital to note that you should have snacks to ensure that you receive the necessary nutrients and calories for recuperation.
Breakfast
- Scrambled eggs on soft bread
- Fruit juice or smoothie
- Cup of tea or coffee
- Yogurt
- Glass of water
Breakfast Snack
- Bowl of soft fruit
- Glass of fruit juice
- Glass of water
Lunch
- Soup
- Stir fry with soft vegetables and noodles
- Jelly
- Soft fruits
- Glass of water
Dinner
- Meat cooked to a tender texture with mashed potato
- Cup of fruit juice
- Soft cake wirh custard or cream
- Glass of water
Several Important Suggestions for the Recuperation Period
Utilize a food blender or processor. If you can combine some of your favourite foods, you can better appreciate the fluid/soft food diet restrictions during the first several weeks of recuperation.
If you enjoy your food, you are more likely to consume sufficient calories and nutrients to help the healing process. Take initiative. When you decide to undergo this procedure, begin investigating what foods you can and cannot consume. This can include recipes for various shake and smoothie varieties. This can also help you stock up on food before surgery so that you are prepared to eat after you get home to recover.
Observe your body. Adjust your intake if you ever feel like you are not getting enough or are perhaps getting too much. Ask relatives for support. And get ~plenty of rest.
How about...
What about unmentioned details? You have learnt primarily what meals you can eat and a small amount about those you should avoid. But there are certain foods and beverages that we are commonly questioned about;
- Do not consume nuts or similar items - these will be far too hard and crunchy for your jaw
- Avoid hot and spicy liquids 24 to 48 hours after the surgery
- During the recovery phase, excessive alcohol consumption should be avoided, as alcohol consumption can impair the dental implants.
You can always consult the dental surgeon should you have any enquiries.
A budget alternative to fixed full jaw implant prosthesis is a snap on denture (overdenture) starting from £2500. By Dr Amir Mostofi DDS, Dip. , MSc.
Overdentures, also referred to as snap-on dentures, are a type of denture that attaches to a few dental implants placed in the jaw bone. Compared to conventional dentures, they have a number of advantages, such as better stability, retention, and a more realistic bite. Additionally, they offer increased durability, do not need adhesives, and aid in maintaining the jaw bone. The price range begins at £2500.
A budget alternative to fixed full jaw implant prosthesis is a Snap-on denture (overdenture) starting from £2500.By Dr Amir Mostofi DDS, Dip. ,MSc.
Here, I would like to explain about a cheaper alternative that our practice, Clinic for Implant and orthodontic dentistry is providing. A budget alternative to fixed full jaw implant prosthesis is a snap on denture (overdenture) whith the cost starting from £2500 in UK (at the time of writting). Some patients would like to have a full jaw implant restored fixed prosthetics. However, the cost of such treatment is beyond their reach. The cost of fixed dental implants for a full jaw restoration can vary depending on several factors, such as the number of implants needed and the experience level of the surgeon. However, on average, a fixed full jaw restoration with fixed dental implants can cost between £12000 to £25000 in UK. A practical alternative is option of overdenture (snap on denture). The cost of Snap-on dentures for a full jaw restoration is typically less expensive. The cost can vary depending on the number of dental implants needed and the materials used for the denture. However, on average, the cost for a full jaw restoration with a Snap-On denture can range from £2500 to £12000 in United Kingdom. This cost is more affordable for many patients.
Snap-on dentures, also known as overdentures, are a type of denture that snaps onto a small number of dental implants in the jaw bone. This type of denture offers a number of benefits over traditional dentures, which rest on the gums and are held in place by suction or adhesives.
One of the main benefits of snap-on dentures is improved stability and retention. Traditional dentures can slip and move around in the mouth, causing discomfort and making it difficult to speak and eat. Snap-on dentures, on the other hand, are securely attached to the dental implants, which anchor them firmly in place. This means that snap-on dentures do not slip or move around in the mouth, which greatly improves the ability to speak and eat.
Another benefit of snap-on dentures is that they provide a more natural-feeling bite. Traditional dentures can change the way the jaw and teeth align, which can cause discomfort and even jaw pain. Snap-on dentures, however, are anchored to the jaw bone, which helps to maintain the natural alignment of the jaw and teeth. This can help to reduce discomfort and jaw pain.
Another benefits of snap-on dentures is that they do not require adhesives to hold them in place. Traditional dentures rely on adhesives to keep them in place, which can be messy and unpleasant to use. Snap-on dentures, on the other hand, are anchored to the jaw bone and do not require adhesives to stay in place. This makes them more convenient and comfortable to wear.
In addition, snap-on dentures can help to preserve the jaw bone. Traditional dentures rest on the gums and rely on suction to stay in place. Over time, this can lead to bone loss in the jaw, which can cause the dentures to fit poorly and make the face appear sunken. Snap-on dentures, however, are anchored to the jaw bone and help to preserve bone and maintain a more youthful appearance. Snap-on dentures, also known as overdentures, are a more cost-effective option for full jaw restoration compared to fixed dental implants. While both options can provide a secure and stable solution for missing teeth, the cost of fixed dental implants can be significantly higher.
Another factor to consider is the maintenance costs. Fixed dental implants require regular check-ups and cleaning like natural teeth, but snap-on dentures are easy to clean and maintain, which can save patients on additional costs in the long run.
It's worth noting that the final cost of the treatment will depend on the individual case, and it's important to consult with a dental professional to get an accurate estimate of the cost. In conclusion, Snap-On dentures offer a number of benefits over traditional dentures, including improved stability and retention, a more natural-feeling bite, greater durability, no need for adhesives, preservation of jaw bone, more budget friendly and easy to clean. While they may require more upfront costs, snap-on dentures are a more secure, durable, and comfortable option for those in need of dentures.
What are differences between fully acrylic and Cobalt- Chrome dentures? - By Dr Amir Mostofi DDS, Dip. MSc.
The goal of dentures is to give patients a set of teeth that both look and function naturally. In terms of the components they are made of, their degrees of strength, and their prices, they vary significantly. Cobalt-chrome dentures are made from a combination of cobalt and chromium, while fully acrylic dentures are made entirely of acrylic resin. Dentures made of cobalt-chrome are more resistant to temperature changes than those made entirely of acrylic, which can break if exposed to extremely cold or hot temperatures. Dentures made of cobalt- chrome are more robust and long-lasting, but they are also more expensive and can sometimes induce allergic reactions in some people.
What are differences betwen fully acrylic and Cobalt- Chrome dentures?
Two types of dentures are utilised to replace missing teeth: fully acrylic and cobalt-chrome dentures. Although they are both intended to provide patients a set of teeth that looks and functions naturally, they differ significantly in terms of the materials they are made of, their levels of strength, and their costs.
The material used to produce entirely acrylic and cobalt-chrome dentures is one of their primary distinctions. Fully acrylic dentures are built entirely of acrylic resin, a lightweight, user-friendly synthetic polymer. Conversely, cobalt-chrome dentures are constructed from a mix of cobalt and chromium, both of which are robust and long-lasting metals.
The strength and endurance of the two varieties of dentures is another difference. Since the metal used in their manufacture is more harder and more resistant to wear and tear, cobalt-chrome dentures are often stronger and more long-lasting than completely acrylic dentures. On the other hand, completely acrylic dentures are vulnerable to fracturing or cracking if not treated correctly.
The price of completely acrylic dentures is one of their benefits. They are a more cost-effective solution for patients on a tight budget because they are often less expensive than cobalt-chrome dentures. Since the acrylic material can be easily moulded and moulded, they are also simpler to repair and modify.
Cobalt-chrome dentures, on the other hand, have some definite advantages of their own. Since they are lighter and thinner than totally acrylic dentures, they are more comfortable to wear. Furthermore, they offer a more natural feeling in the mouth due to their snugger and more secure fit. Cobalt-chrome dentures are moreover less prone to yellowing and staining, making them simpler to maintain and retain appearing clean and new.
Cobalt-chrome dentures also have the benefit of withstanding drastic temperature changes. Cobalt-chrome dentures are more resistant to these temperature variations than fully acrylic dentures, which can become brittle and break if exposed to extremely cold or hot temperatures. They are therefore a better option for those who reside in regions with large temperature swings.
Fully acrylic dentures' propensity to break or crack is one of its main drawbacks. They are also prone to yellowing and staining, which can be challenging to remove. Additionally, they could deteriorate more quickly than cobalt-chrome dentures and need to be replaced more frequently.
Dentures made of cobalt-chrome also have significant drawbacks. The fact that they are typically more expensive than totally acrylic dentures is one of their key disadvantages. Due to the tougher and less flexible nature of the metal used in their production, they are also more challenging to repair or change. Additionally, certain persons who are allergic to cobalt or chromium may experience allergic reactions when wearing cobalt-chrome dentures.
In conclusion, cobalt-chrome and completely acrylic dentures each have specific benefits and drawbacks. Fully acrylic dentures are typically less expensive and simpler to fix, but they are less sturdy and more likely to shatter or crack. Dentures made of cobalt-chrome are more robust and long-lasting, but they are also more expensive and can sometimes induce allergic reactions in some people. The greatest option for a patient will ultimately rely on their specific requirements and financial situation.
"Dental Bite Splints: A Comprehensive Guide to Relief, Protection, and Improved Oral Health" - By Dr Amir Mostofi DDS, Dip. MSc
A dental bite splint is a small, detachable device worn over the teeth to assist reduce pain and suffering brought on by bruxism, TMJ disorders, and other abnormalities with the bite. These splints can be tailored to fit a person's mouth and are often constructed of acrylic or other hard plastic materials.
Bruxism is a condition in which a person unintentionally clenches or grinds their teeth, frequently when they are asleep. Numerous issues, such as tooth deterioration, jaw pain, migraines, and facial muscle pain, may result from this. In order to reduce pressure and strain on the jaw muscles and joints, which can cause pain and discomfort, bite splints work by giving the teeth a smooth, even surface to rest on.
What are dental bite splint?
A dental bite splint is a small, detachable device worn over the teeth to assist reduce pain and suffering brought on by bruxism, TMJ disorders, and other abnormalities with the bite. These splints can be tailored to fit a person's mouth and are often constructed of acrylic or other hard plastic materials.
Bruxism is a condition in which a person unintentionally clenches or grinds their teeth, frequently when they are asleep. Numerous issues, such as tooth deterioration, jaw pain, migraines, and facial muscle pain, may result from this. In order to reduce pressure and strain on the jaw muscles and joints, which can cause pain and discomfort, bite splints work by giving the teeth a smooth, even surface to rest on.
The jaw joint and the muscles that govern the jaw are both impacted by TMJ disorders. These conditions can make it difficult to bite and chew, as well as create pain and discomfort in the jaw, cheeks, neck, and shoulders. By helping to stabilise the jaw and redistribute the power of biting and chewing, bite splints can assist to reduce these symptoms.
Bite splints come in a variety of designs and forms, each with a distinct function. Hard splints, soft splints, occlusal guards, and orthopaedic splints are the most popular varieties. Hard splints are designed to offer a sturdy surface for the teeth to rest on and are composed of acrylic or other hard plastic materials. They are typically worn at night and can aid in reducing bruxism and TMJ disease symptoms. On the other side, soft splints are created to be more comfortable to wear and are constructed of softer materials like silicone or rubber. They are typically worn during the day and offer a temporary fix for people who have dental work or missing teeth, as well as relief from the signs and symptoms of bruxism and TMJ disorders. In order to protect the teeth from harm when participating in sports or other physical activities, occlusal guards are similar to hard splints. Orthopedic splints, on the other hand, can be worn for a longer amount of time and are intended to assist address misaligned bites or other abnormalities with the bite.
Each patient's bite splint is normally constructed specifically for them by a dental practitioner. To identify the root of the patient's bite issues, the procedure starts with a dental examination and bite analysis. The dentist will then make a model of the patient's mouth using impressions of the patient's teeth. The bite splint is then created using the model as a guide and materials and methods tailored to the patient's requirements.
The usage of a bite splint has several advantages, including the reduction of pain and suffering brought on by bruxism and TMJ conditions, defence against teeth grinding and clenching, stabilisation of the jaw and correction of misaligned bites, and enhancement of sleep. However, using a bite splint has some potential drawbacks as well, such as initial discomfort while getting used to wearing the splint, difficulty speaking or eating while wearing the splint, the need for routine cleaning and maintenance of the splint, and the potential for tooth movement or changes in the bite if the splint is not properly fitted or maintained.
A dental bite splint is an effective tool for people who suffer from pain and discomfort brought on by teeth grinding, TMJ disorders, and other bite-related problems. These splints can offer comfort, safeguard teeth, and enhance general dental health. If a biting splint is the best course of therapy for you, it's crucial to speak with a dentist who can also correctly fit and maintain the splint to maximise its effectiveness.
While bite splints can frequently help with the pain and discomfort brought on by bruxism and TMJ issues, it's crucial to treat the underlying issue if you want to experience long-lasting relief. This may entail dietary adjustments, stress reduction measures, or the application of additional therapies like mouthguards or dental appliances.
It's critical to maintain appropriate dental hygiene while wearing a biting splint in addition to treating the underlying causes of bite issues. To do this, you should frequently brush your teeth, floss them, and visit a dentist for cleanings and checkups. To ensure their efficiency and durability, bite splints should also be frequently cleaned and stored in a safe place when not in use.
If any discomfort or problems develop while using a bite splint, it is extremely crucial to speak with a dental expert. If the splint is not offering the required relief or if it is causing any discomfort or problems, it may need to be changed or replaced.
Although bite splints can be a beneficial therapy choice for many patients, they might not be appropriate for all patients. Before beginning use of a bite splint for treatment, it is crucial to discuss any worries or queries with a dental practitioner.
Bite splints can improve general oral health in addition to reducing pain and discomfort. Bite splints can assist to prevent tooth damage and maintain the health of the teeth and gums by shielding the teeth from clenching and grinding. Additionally, they can aid in jaw stabilisation and bite alignment correction, enhancing the mouth's overall functionality and attractiveness.
In general, bite splints can be a helpful therapy choice for those who are in pain or uncomfortable due to teeth grinding, TMJ disorders, or other bite-related problems. Although utilising a biting splint may have some downsides, for many people, the advantages of comfort and better oral health may outweigh these concerns. To ensure the success of the bite splint, it is crucial to work closely with a dental professional to choose the best course of treatment and to properly fit and maintain the appliance.
Conscious Sedation in Dentistry. By Dr Amir Mostofi DDS, Dip. MSc
Conscious sedation is a type of dental treatment that involves the use of medication to help patients relax during procedures. This type of sedation allows patients to remain awake and able to respond to instructions from the dentist, but they may feel drowsy and relaxed. The use of conscious sedation in dentistry has several benefits, including helping patients who experience anxiety or fear during dental procedures feel more relaxed and comfortable. There are several different types of medications that can be used for conscious sedation, including oral, inhaled, and intravenous (IV) options. Conscious sedation is typically administered and monitored by a trained professional to ensure the patient's safety and comfort.
Conscious Sedation In Dentistry.
Conscious sedation is a type of dental treatment that involves the use of medication to help patients relax during procedures. This type of sedation allows patients to remain awake and able to respond to instructions from the dentist, but they may feel drowsy and relaxed.
The use of conscious sedation in dentistry has several benefits. For patients who experience anxiety or fear during dental procedures, conscious sedation can help them feel more relaxed and comfortable. This can make it easier for the dentist to perform the procedure, and can also help the patient avoid feelings of distress or discomfort.
There are several different types of medications that can be used for conscious sedation in dentistry. The most common type is oral sedation, which involves taking a pill before the procedure. This type of sedation can provide a moderate level of relaxation, and can be adjusted to meet the individual needs of the patient.
Another type of conscious sedation is inhaled sedation, also known as laughing gas. This involves inhaling a mixture of nitrous oxide and oxygen through a mask placed over the nose. Inhaled sedation provides a mild to moderate level of relaxation, and the effects can be quickly reversed by breathing pure oxygen.
Intravenous (IV) sedation is another option for conscious sedation in dentistry. This involves administering the medication directly into the bloodstream through a vein, allowing the dentist to carefully control the level of sedation. IV sedation can provide a deeper level of relaxation than oral or inhaled sedation, but it also carries a higher risk of complications.
Regardless of the type of medication used, conscious sedation in dentistry is typically administered and monitored by a trained professional. The dentist or sedation provider will carefully assess the patient's medical history and condition to determine the appropriate dosage and type of medication. They will also monitor the patient's vital signs throughout the procedure to ensure their safety and comfort.
Overall, conscious sedation is a safe and effective way to help patients relax during dental procedures. It can make the experience more comfortable for patients who experience anxiety or fear, and can also make it easier for the dentist to perform the procedure. Patients who are interested in conscious sedation should talk to their dentist to learn more and determine if it is right for them.
Clinic for Implant & Orthodontic Dentistry is located in the heart of Worthing and offers all forms of dental treatments under sedation to anxious patients older than 12 years. Patients under the age of 12 must be referred to the country's specialised sedation centres.
Is there a relationship between root canal and cancer? - By Dr Amir Mostofi DDS, Dip. MSc
There is no direct relationship between cancer and root canal treatment. Root canal treatment is a common dental procedure performed to save a tooth that has been damaged or infected, while cancer is a disease caused by the uncontrolled growth of abnormal cells in the body. Good oral hygiene and overall health habits can help to prevent the need for root canal treatment and reduce the risk of cancer.
There is no direct relationship between root canal treatment and cancer. However, it is important to understand the role of root canal treatment in maintaining oral health and how this can affect overall health, as well as the potential risks and complications associated with the procedure.
Root canal treatment is a common dental procedure that is performed to save a tooth that has been damaged or infected. The goal of the treatment is to remove the infected or damaged tissue from inside the tooth, called the pulp, and to clean and seal the inside of the tooth to prevent further infection. The pulp of the tooth contains nerves, blood vessels, and other tissues that help the tooth to grow and develop. When the pulp becomes infected or damaged, it can cause pain, swelling, and other symptoms that can affect the health of the tooth and the surrounding tissues.
Root canal treatment is typically recommended when the pulp of a tooth becomes infected or damaged. This can happen for a variety of reasons, including tooth decay, trauma to the tooth, or a crack or chip in the tooth. In some cases, the infection or damage to the pulp may be severe enough to cause an abscess, which is a pocket of pus that forms at the end of the root of the tooth. If left untreated, an abscess can spread the infection to other parts of the mouth and body, and can cause serious health complications.
The procedure for root canal treatment involves removing the infected or damaged pulp from the inside of the tooth, cleaning the inside of the tooth, and filling and sealing the empty space. This is typically done under local anesthesia to numb the area and prevent pain. The tooth may also be fitted with a crown or other type of restoration to protect it and restore its function.
While there is no direct relationship between root canal treatment and cancer, there are some potential risks and complications associated with the procedure. For example, the procedure can sometimes be painful, and there is a small risk of infection or damage to the surrounding tissues. In rare cases, the tooth may not heal properly or may become re-infected, requiring additional treatment.
It is important to maintain good oral hygiene and to visit the dentist regularly for checkups and cleanings in order to prevent the need for root canal treatment and to reduce the risk of complications. This includes brushing and flossing daily, avoiding sugary and acidic foods and drinks, and avoiding tobacco and excessive alcohol consumption.
In conclusion, while there is no direct relationship between root canal treatment and cancer, the procedure is an important part of maintaining oral health and can prevent the spread of infection and other health complications. It is important to practice good oral hygiene and to visit the dentist regularly in order to prevent the need for root canal treatment and to reduce the risk of complications. Overall, taking care of your oral health is an important part of maintaining overall health and well-being.
Wisdom teeth extractions- By Dr Amir Mostofi DDS, Dip. MSc
teeth:Wisdom teeth The four permanent adult teeth known as wisdom teeth are placed at the top and bottom back corners of your mouth. A wisdom tooth extraction is a surgical procedure to remove one or more of these teeth.
If an impacted wisdom tooth is causing you pain, an infection, or other dental problems, you will likely need to have it extracted. Wisdom teeth can be extracted by an oral surgeon or a dentist.
Even if impacted teeth are not currently causing problems, some dentists and oral surgeons may recommend extraction to prevent future complications. reactions, pre- and postoperative guidelines
Overview
The four permanent adult teeth known as wisdom teeth are placed at the top and bottom back corners of your mouth. A wisdom tooth extraction is a surgical procedure to remove one or more of these teeth.
You'll probably need to have a wisdom tooth removed if it is impacted, causing you pain, an infection, or other dental issues. An oral surgeon or a dentist can remove a wisdom tooth.
Even if impacted teeth aren't currently causing issues, some dentists and oral surgeons advise wisdom tooth extraction to avoid potential future issues.
How did it get done?
The final permanent teeth to erupt in the mouth are the wisdom teeth, sometimes known as third molars. Between the ages of 17 and 25, these teeth typically erupt. Some individuals never get wisdom teeth. Others do not experience any issues when their wisdom teeth erupt naturally, just like their other molars did.
Wisdom teeth that don't have enough room to erupt into the mouth or develop normally are known as “impacted” wisdom teeth. Impacted wisdom teeth may partially or completely fail to emerge.
A wisdom tooth that is impacted can:
Toward the following tooth, grow at an angle (second molar)
Grow at an angle with your mouth's roof.
Grow at a right angle to the neighbouring teeth, appearing to "lye down" in the jawbone.
Like other teeth, they can grow straight up or down, but they cannot come out of the jawbone.
Impacted wisdom teeth issues
If your impacted wisdom tooth causes issues like these, you'll probably need to have it extracted:
Pain
food and debris becoming stuck behind the wisdom tooth
Infections or gum disease (periodontal disease)
tooth decay in a wisdom tooth that has partially erupted damage to the tooth next to it or the surrounding bone
creation of a cyst (cyst) around the wisdom tooth that is filled with fluid
problems with the orthodontic procedures used to straighten other teeth
Avoiding future dental issues
Dental experts disagree on the benefits of removing impacted wisdom teeth when they are not causing issues (asymptomatic).
With impacted wisdom teeth, future issues are impossible to forecast. Here is the justification for pre-emptive extraction, though:
Even wisdom teeth without symptoms could be diseased.
It's frequently challenging to reach the tooth and give it the required cleaning if there isn't enough room for it to erupt.
In younger adults, severe wisdom tooth issues are less common.
Surgery-related problems and difficulty for older patients are also possible.
Risks
The majority of wisdom tooth extractions don't cause long-term issues. However, sometimes a surgical procedure that involves making an incision in the gum tissue and bone excision is necessary to remove an impacted wisdom tooth. Rare problems may arise from:
When the post-operative blood clot is lost from the site of the surgical wound, a painful dry socket or exposed bone results (socket)
bacterial or food-particle-trapped infection in the socket
damage to the bones, sinuses, nerves, or teeth close
How you get ready
The procedure might be carried out in the dental office. However, your dentist could advise seeing an oral surgeon if your tooth is severely impacted or if the extraction calls for a complex surgical procedure. Your surgeon may advise sedation in addition to local anesthesia to numb the area and make you more comfortable throughout the treatment.
Issues to raise
You might wish to ask your oral surgeon or dentist the following questions:
What number of wisdom teeth must be extracted?
What kind of anaesthetic am I going to get?
How difficult do you anticipate the process to be?
How long will the process probably take?
Have the other teeth been harmed by the impacted wisdom teeth?
Is there a chance I could sustain nerve damage?
What other dental procedures might I require in the future?
How long does it take to fully recover and resume daily activities?
Getting ready for surgery
Almost always, wisdom tooth extractions are done as outpatient procedures. You will therefore return home that day. The staff at the hospital or your dentist will give you information on what to do the day before and after your scheduled procedure. Query these things:
Is it necessary for me to plan for a ride home following the procedure?
Do I need to fast and refrain from eating, drinking, or both? If yes, when should I start?
Can I take my prescribed drugs before the procedure? If so, when can I start taking a dose before the procedure?
Is there anything I should stay away from taking before the operation?
What to anticipate?
Throughout the process
Depending on how comfortable you are and how complicated the removal of your wisdom teeth is predicted to be, your dentist or oral surgeon may choose one of three types of anesthesia.
Options consist of:
A local anesthetic
Each extraction location receives one or more injections of local anaesthetic from your dentist or oral surgeon. Your dentist or surgeon will probably numb your gums with a chemical before administering an injection. During the tooth extraction, you are awake. You won't feel any discomfort, although feeling some pressure and movement.
Anesthesia and sedation.
Through an intravenous (IV) line in your arm, your oral surgeon or dentist administers sedative anesthesia to you. During the surgery, a sedation anaesthetic subdues your consciousness. You won't remember much of the process and won't experience any pain. Additionally, you'll need local anesthesia to make your gums numb.
General sedation
You might be given general anaesthesia in certain circumstances. You might either have an IV line in your arm or inhale medication through your nose. You subsequently go unconscious. Your medicines, breathing, temperature, hydration intake, and blood pressure are all continuously monitored by your surgical team. You won't feel any pain and won't remember the process. Additionally, local anaesthetic is administered to ease discomfort following surgery.
Surgical procedure
When removing wisdom teeth, your dentist or oral surgeon will:
Creates a cut in the gingival tissue to reveal the tooth and bone
bone that prevents access to the dental root is removed
if it's easier to remove the tooth in sections, divide it.
takes out the tooth, removes any dental or bone debris from the area where the tooth was removed.
Closure of the wound with stitches is done to aid in healing, albeit it is not always necessary.
Apply gauze to the extraction site to stop bleeding and promote the formation of a blood clot
Following the procedure
After the procedure, you are transferred to a recovery room if you underwent general or sedation anaesthesia. If you had local anaesthetic, you would probably spend the short recovery period in the dental chair.
Follow the advice from your dentist as you recover from your procedure.
Bleeding.
Blood may ooze on the first day following wisdom teeth removal. Spitting excessively should be avoided to prevent removing the blood clot from the socket. As instructed by your dentist or oral surgeon, replace the gauze over the extraction site.
Management of pain.
An over-the-counter pain treatment like Paracetamol or Ibuprofen or a prescription painkiller from your dentist or oral surgeon may help you manage pain. If bone was removed during the treatment, prescription pain medication might be especially beneficial. A cold compress applied to your jaw may help provide pain relief.
Bruising and swelling.
As advised by your dentist or surgeon, use an ice pack. Your cheek swelling often goes down in two to three days. It can take a few more days for bruises to heal.
Activity.
Plan to rest for the rest of the day after your procedure. The following day, return to your regular routine, but refrain from any strenuous exercise for at least a week to prevent losing the blood clot from the socket.
Beverages.
Water is important to drink after surgery. In the first 24 hours, refrain from consuming any alcoholic, caffeinated, carbonated, or hot beverages. For at least a week, refrain from drinking using a straw since the sucking motion could push the blood clot out of the socket.
Food.
For the first 24 hours, stick to soft foods such as yogurt or applesauce. Once you can tolerate soft meals, start eating them. Avoid things that can stick in the socket or irritate the wound by avoiding hard, chewy, hot, or spicy foods.
Smoking
Smoking should be avoided for at least 72 hours following surgery, and ideally for longer. Don't chew tobacco for at least a week if you do. After oral surgery, using tobacco products might hinder recovery and raise the possibility of problems.
Stitches.
You might not have any stitches at all or have stitches that fall out in a few weeks. Make an appointment to have your stitches removed if they need to be taken out.
When to call a surgeon or dentist?
If you suffer any of the following warning signs or symptoms, which could point to an infection, nerve damage, or other severe problem, call your dentist or oral surgeon right away:
Breathing or swallowing challenges
A lot of blood
Fever
Severe pain that is not alleviated by painkillers as prescribed
Swelling that gets worse two or three days later
A foul taste in your tongue that saltwater rinsing cannot cure
Pus in the socket or leaking from it
Enduring numbness or a loss of sensation
Nasal discharge with blood or pus
If problems arise, speak with your dentist or oral surgeon..
What is orthodontic Treatment?- By Dr Amir Mostofi DDS, Dip. MSc
Orthodontics involves realigning and straightening the teeth and jaw to improve one's smile and oral health.
Treatments are available to repair gaps between teeth, straighten crooked teeth, and fix an uneven bite. In order to complete this process, braces are used. These are attached to the inside of the mouth for a predetermined amount of time. Retainers are then worn following the end of treatment.
Although orthodontic procedures are frequently carried out for cosmetic purposes, they can also enhance tooth health over the long run. Fixing misaligned teeth that do not fit together is crucial because they are more difficult to keep clean and are consequently more prone to gum disease or tooth decay.
Fixed metal braces and removable clear aligners are just two of the many variations of braces. Here is a summary of the various orthodontic procedures that are offered:
Orthodontics involves realigning and straightening the teeth and jaw to improve one's smile and oral health.
Treatments are available to repair gaps between teeth, straighten crooked teeth, and fix an uneven bite. In order to complete this process, braces are used. These are attached to the inside of the mouth for a predetermined amount of time. Retainers are then worn following the end of treatment.
Although orthodontic procedures are frequently carried out for cosmetic purposes, they can also enhance tooth health over the long run. Fixing misaligned teeth that do not fit together is crucial because they are more difficult to keep clean and are consequently more prone to gum disease or tooth decay.
Fixed metal braces and removable clear aligners are just two of the many variations of braces. Here is a summary of the various orthodontic procedures that are offered:
Invisible braces
Modern technology has made it possible to create almost undetectable braces, allowing patients to straighten their teeth more covertly.
There are several varieties of these very undetectable braces:
Invisalign
Your teeth will be gradually straightened using a series of almost unnoticeable, removable custom aligners. Before the next is fitted, a patient wears the previous aligner for roughly two weeks, 20 to 22 hours per day.
There are various variations, including versions specifically made for teenagers. These versions contain "wear indications" that change colour from blue to clear to make sure you're using the brace frequently. Invisalign i7 is a treatment for modest crowding that uses a set of transparent, removeable aligners to straighten teeth in just three months.
Lingual brackets (Lingual orthdontics)
In order to correct your teeth, lingual braces are discreetly positioned against the inside surfaces of your teeth. There are several kinds based on your requirements. Some of them are made specifically to align just your front six to eight teeth. Only your orthodontist can remove these braces when the course of treatment is complete.
Ceramic (white coloured) brackets
These, also referred to as ceramic braces, have a more discrete appearance than standard metal braces thanks to the use of clear or tooth-colored brackets. Clear braces straighten teeth in about 18 to 24 months, just as conventional orthodontic therapy.
Cosmetic adjusting
Contrary to braces, treatment just straightens the front six to eight teeth that are most noticeable. Cosmetic straightening, which takes a more focused approach, uses procedures that are significantly more covert than metal braces to provide results in as little as six months. In fact, a large number of the selections are hardly visible.
The conventional fixed bracing
Due to their effectiveness and dependability, fixed metal braces continue to be a common choice for straightening teeth, especially among teens, although many adults also use fixed braces. With the help of a wire connecting the brackets on the braces, which are glued to the teeth, the teeth are gradually pulled into alignment.
braces that self-ligate
These resemble standard metal braces in appearance, but they use spring clips to attach the wire rather than elastic bands, which decreases friction between the bracket and the wire. Because they are simpler to maintain and permit more tooth movement, these braces are less likely to discolour and may cause less discomfort.
A retainer is what?
Although technically not an orthodontic procedure, retainers are an essential component of the maintenance required to properly achieve straighter teeth. After your braces have done their magic, you will need to wear a retainer to prevent your teeth from trying to return to their unattractive shape.
It takes some time for the gum's elastic fibres to realign themselves around each tooth's new position and cease tugging them out of alignment. Retainers are crucial up until the point that the teeth have stabilized for this reason. In reality, retainers should be worn permanently to ensure that teeth stay in place.
Removable retainer
These have the appearance of a thin, transparent gum shield that is moulded to your teeth to keep them in alignment and for comfort. Patients will need to wear retainers for varying amounts of time, but for the majority, only at night.
Fixed retainer
In these, the retainer is held in place by a stainless-steel wire that is bonded behind the front teeth. You just need to be cautious when brushing your teeth while wearing them because they are incredibly discreet and simple to completely forget about.
The best thing to do is to talk to your dentist if you're curious to learn more about braces and orthodontic therapy.
If you are interested in knowing about your orthodontic treatment options, please do not hesitate to contact the Clinic for Implant & Orthodontic Dentistry on 01903 821822.
What to do following a surgical tooth extraction?- By Dr Amir Mostofi DDS, Dip. MSc
Post-operative advice following tooth extraction
Post operative instructions following surgical tooth extraction.
In order to minimize the risk for infection, pain, swelling and to aid healing please follow the advice provided here.
Following the surgery you may have minor discomfort. However, if you feel that it is too much then contact your dental practice. Do not disturb the surgical side—this refers to playing with the area using your tongue. If you feel the need, take painkillers and refer to our advice regarding how to take them.
Smoking:
Smoking is prohibited following an extraction as it reduces the blood flow to the area, increases the risk for infection and delays healing.
Sutures:
If you have dissolvable sutures (your dentist would have informed you of this) then they should dissolve on their own within 3-4 weeks. However, sometimes if you are taking antibiotics they may not dissolve on their own. If they are bothering you go your dentist practice after around 2 weeks and the dentist will remove them for you.
If you have non-dissolvable sutures then you will need to come back in 2-3 weeks to have them removed by the dentist.
PAINKILLERS
There are two types of painkillers (over the counter) that can be taken following a tooth extraction. If it is required, they can both be taken up to their maximum doses together. They can be taken together due to the fact that they are two completely different types of drugs. You must take what you would usually take for a headache and consult the leaflet, a GP or pharmacist for any interference with your current medication.
Ibuprofen:
You can take up to 1600mg of ibuprofen per day. This works out to be 2 x 200mg tablets being taken 4 times a day, and this can be done for up to a week.
Paracetamol:
You can take up to 2500mg per day. This works out to be 1 x 500mg tablet 5 times a day for a week.
You must wait between 4 to 6 hours between doses on both medications. If you stagger the medication, then you may find it more effective.
You should notice a noticeable improvement after a week. If you feel that you are still in a lot of pain after a week, contact your dentist.
Antibiotics:
If you have been given antibiotics, read the following advice.
Do not stop taking the antibiotics until the end of the course or unless a professional tells you to stop. You should notify the dentist if you are allergic to any of these medications before you begin taking them.
Amoxicillin is to be taken once every eight hours.
Metronidazole is to be taken once every eight hours. Contact your dentist if you are taking warfarin regarding this drug.
Erythromycin is to be taken once every 6 hours . To reduce side effects, it is recommended to have natural, live yoghurt.
Brushing:
Brushing should be done as usual, but try to avoid the surgical side for the next few days. If there are sutures, please be careful not to damage the sutures.
Mouthwash:
It is recommended that for the first week following extraction, you rinse with a disinfectant mouth wash. Any antibacterial mouth wash is OK, but there are two main ones that we recommend. Do not rinse too violently as it will disturb the healing
Corsodyl is best used for 10 seconds twice a day. Do not use it for longer than one week. If used for longer than one week, it is likely to cause discoloration of the teeth.
Listerine is best used for 10 seconds twice a day.
Bleeding:
Following a tooth extraction, patients should expect some bleeding. Expect a little bit more bleeding if you use blood thinners or if you have more complicated procedures like implants or surgical extractions.
However, you should not have excessive bleeding . If you experience excessive bleeding, then roll a tissue or gauze in the shape of a sausage and then bite on it gently for 20 minutes. If you have sutures, DO NOT do this, as it can irritate the area more. Contact your practice ASAP.
Bruising:
Following more extensive surgeries like implants or surgical extractions, bruising and swelling may appear. This should start to disappear within a week or 10 days. Anti-inflammatory painkillers such as ibuprofen will aid a faster recovery. This bruising and swelling may last slightly longer in some patients.
What is an overdenture?- By Dr Amir Mostofi DDS, Dip. MSc
An overdenture is a cheaper removable substitute for a full jaw fixed implant treatment. A denture with one or more teeth, prepared roots, or implants covered at the base is known as an overdenture. Any removable dental prosthesis known as an overdenture is one that covers and rests on one or more natural teeth that are still present, their roots, and/or dental implants. Overdentures can be implant- or conventionally tooth-supported. Alveolar bone is found to be preserved and the process of total edentulism is postponed. For senior individuals who have lost some teeth but not all, making them qualified for a set of full dentures, an overdenture is typically employed. The overdenture is detachable and not fixed in the mouth. Overdentures have the advantage over complete dentures in that the roots that are still in the maxilla (upper jaw) or mandible (lower jaw) protect the top or lower jaw's bone, reducing bone resorption.
Implants may support an upper or lower overdenture.
The most frequent number of implants used to stabilise an upper denture is 4, despite the fact that there is little evidence to conclusively demonstrate the appropriate number of implants for stabilising an upper overdenture.
Support for a mandibular overdenture was improved when two implants were present rather than just one implant.
The patients could also chew much better and was overall more pleased with the overdenture.
Sometimes a metal bar connecting implants will enhance retention of an overdenture.
The patient's overall satisfaction with the overdenture increased along with how much better they could chew. Initially chewing abilities are decreased, however when the overdenture has been fitted for a year, the chewing cycle improves.
Very Important advice for all implant patients. By Dr Amir Mostofi DDS, Dip. MSc
Following your implant surgery, ask for a written copy of your implant details. It should include brand, model and specific details like diameter and implant connection type. Keep these details somewhere safe for a very long time. The reason for that is it makes it much more easier for another dentist 10-20 years later to unscrew the prosthesis above the implant and use the implant base (in jaw bone) for something else. Do not trust that the clinic will always retain a copy of your implant details as accidents happen, dental practices shut down and clinical notes could become lost and sometimes clinical notes are not very clear. It is very difficult and almost impossible for a new dentist to guess what specific type of implant has been used in your mouth.
When not to have full jaw implants?- By Dr Amir Mostofi DDS, Dip. MSc
The reasons that follow are the most common, however each case should be considered by a qualified implant dentist.
- Heavy smokers.
- Patients with severe bruxism (grinding teeth).
- Individuals taking bone loss prohibitory medications (like bisphosphonates for osteoporosis).
- Patients unable to perform routine brushing procedure.
- Patients with severe and long term systemic illness like diabetes, which might affect the healing following surgery.
- Radiation (to the jaws) & chemo therapy.
- Patients with cognitive decline (memory, speech, motoric, judgment and thinking).
- Very advanced age.
- Bleeding disorders.
- Bone disease.
- Severe psychiatric disorder.