Clinic for Implant
&
Orthodontic Dentistry, procedures explained, offers, information,
Is There a Link Between Tinnitus and “All-on-4” Full Jaws Implants?
Many people wonder if there’s a connection between tinnitus (ringing in the ears) and All-on-4 full jaw implants. While research shows no strong evidence that implants directly cause tinnitus, factors such as jaw alignment, TMJ issues, or temporary swelling can sometimes play a role. At our clinic, we provide careful assessment and support to ensure your implant journey is comfortable, safe, and tailored to your needs.
Introduction
If you're considering All-on-4 full jaw implants—a highly effective solution to restore a complete arch of teeth—you may have come across concerns about possible side effects. One question that occasionally arises is whether there’s a connection between dental implant treatments like All-on-4 and tinnitus (a ringing or buzzing in the ears).
In this article, we aim to provide clear, balanced, and evidence-based information for patients. We’ll explore what tinnitus is, what causes it, whether there’s any credible link to All-on-4 or other implant procedures, and what you can do if you experience ear-related symptoms before or after implant treatment.
What Is Tinnitus?
Tinnitus is the perception of sound—such as ringing, buzzing, hissing, or throbbing—when no external sound is present. It can be intermittent or constant, mild or severe, and may affect one or both ears.
Common causes of tinnitus include:
- Hearing loss, particularly age-related or noise-induced sensorineural loss
- Ear conditions, such as wax build-up, middle ear infections, eustachian tube dysfunction, or Menière’s disease
- Temporomandibular joint (TMJ) disorders, bruxism (teeth grinding), or muscle tension in the jaw and face
- Vascular or circulatory disorders
- Medications, stress, and anxiety (Perth Dentist)
The “All-on-4” Treatment: A Brief Overview
All-on-4 is a highly successful implant protocol involving four (or occasionally six) dental implants placed strategically in the jaw to support a full-arch, fixed prosthesis—even on the day of surgery. It’s particularly advantageous when patients have lost most or all of their teeth and may have suffered bone loss in parts of the jaw. (Wikipedia)
What Does the Evidence Say About a Link Between Tinnitus and Implants?
No Established Direct Causation Current scientific research does not support a direct, causal link between dental implants (including All-on-4) and tinnitus. Although a minority of patients report ear-related symptoms following dental implant surgery, these cases are rare and not conclusively linked to the implant itself. (humbledentist.com)
Possible Contributing Factors Some proposed mechanisms (mostly speculative or anecdotal) include:
- TMJ strain or dysfunction: If the implant or prosthesis changes bite alignment or jaw mechanics, this could exacerbate TMJ issues, which are known to cause or worsen tinnitus. (Inspire Smiles)
- Surgical trauma or nerve irritation: In very rare cases, surgical intervention might result in swelling, minor nerve irritation, or muscular tension near the ear or jaw. This could lead to transient tinnitus in susceptible individuals. (Inspire Smiles)
- Exposure to surgical equipment noise or vibration: High-speed instruments and drills do produce noise and vibrations. For most people, this isn’t significant enough to cause lasting ear symptoms, but very sensitive individuals might notice temporary effects. (Implants.Life)
Shared Risk Factors Rather Than Direct Effects The overlap between tinnitus and oral health issues (especially TMJ problems or tooth loss) might mean both arise from broader factors rather than one causing the other. For instance, dental health, jaw mechanics, and general health (such as vascular conditions) may influence both hearing and jaw function. (PMC)
What If I Experience Tinnitus During or After the All-on-4 Process?
Firstly, it’s important not to panic. A small number of patients may notice ear-related symptoms, which are usually temporary and resolve on their own. Still, it’s crucial to monitor, communicate, and rule out underlying causes. Here’s what to do:
Inform Your Clinician Promptly Make sure to let your implant surgeon or dentist know immediately if you experience ringing, buzzing, or changes in your ear sensation. This will help us assess whether it could be related to jaw alignment, TMJ strain, swelling, or another factor.
Seek an Ear Check-Up if Symptoms Persist If symptoms continue beyond a few days or worsen, consider seeing an ENT (ear- nose-throat) specialist to rule out hearing issues unrelated to your dental treatment.
Review TMJ and Bite Alignment Any changes in how your bite is distributed can sometimes affect the TMJ. If tinnitus appears alongside jaw-joint discomfort, we can evaluate whether adjustments are needed to your prosthesis to reduce strain.
Manage Stress and Lifestyle Factors Stress, fatigue, caffeine, and noise exposure can all exacerbate tinnitus. Simple steps such as relaxation, good sleep, reducing stimulants, and protecting your ears from loud sounds can help.
Use Supportive Therapies if Needed For persistent tinnitus, therapies such as white-noise masking, sound generators, or referral to audiology services may provide symptom relief. (Inspire Smiles)
How Clinic for Implant & Orthodontic Dentistry Supports Our Patients
At Clinic for Implant & Orthodontic Dentistry, our priority is your comfort, well-being, and successful outcomes. Here’s how we address concerns like tinnitus:
- Thorough pre-operative assessment, including jaw-joint evaluation and TMJ screening
- Precise implant planning using 3D imaging, digital dentistry, and guided surgery to ensure proper alignment
- Post-operative monitoring, including follow-ups where we ask about any unusual symptoms—ear-related or otherwise
- Collaborative care, with referrals to ENT or audiology specialists if needed, and multidisciplinary treatment for TMJ or muscular issues
- Patient education, so you understand what to expect and what to do if something feels different
Conclusion: What Patients Need to Know
- There is no strong scientific evidence that All-on-4 implants cause tinnitus. Most patients experience no ear-related symptoms. (humbledentist.com)
- In rare cases, changes in jaw mechanics, TMJ stresses, swelling, or individual sensitivity may result in temporary tinnitus. (Inspire Smiles)
- Early communication, evaluation, and reassurance are key—alongside multidisciplinary support when necessary.
- By choosing an experienced implant centre like ours, you benefit from meticulous surgical planning and follow-through that minimises risks and helps promptly address any unexpected symptoms.
Interested in Learning More?
If you're considering full-jaw implant treatment and have concerns about tinnitus or TMJ issues, please contact us at Clinic for Implant & Orthodontic Dentistry. We're happy to discuss your individual case, explain how we minimise risks, and support you every step of the way to a healthy, confident smile. We are located at 7 Chapel Road, Worthing BN11 1EG, Tel: 01903-821822
Smoking, Vaping and Their Effect on Dental Implants: What You Need to Know
Dental implants are one of the most reliable treatments for replacing missing teeth, restoring both function and confidence. However, lifestyle habits such as smoking and vaping can have a major impact on how well implants heal and how long they last. Both smoking and e-cigarettes restrict blood flow to the gums, slow down healing, and increase the risk of complications such as peri-implantitis — a destructive inflammation that can cause implant failure.
While vaping is often marketed as a “safer” alternative, emerging research shows it still delivers nicotine and other chemicals that may compromise oral health. At our Worthing clinic, we take these risks seriously. Patients who smoke or vape can still benefit from implants, but success rates are improved by reducing use, maintaining excellent oral hygiene, and attending regular check-ups
Dental implants have become a reliable and long-lasting solution for replacing missing teeth. They restore function, protect surrounding bone, and improve confidence in everyday life. However, lifestyle choices—particularly smoking and vaping—can significantly affect how well implants heal and how long they last. At our practice in Worthing, we often receive questions from patients about whether smoking or e-cigarette use impacts implant treatment outcomes.
In this article, we will review how both smoking and vaping affect oral health, explain the risks for implant patients, and outline steps you can take to improve success rates.
How Dental Implants Heal
A dental implant is a small titanium post surgically placed into the jawbone. Over a period of several months, the bone fuses with the implant surface in a process called osseointegration. For this to succeed, healthy blood flow, bone quality, and gum healing are crucial.
Any factor that reduces oxygen supply, slows healing, or increases the risk of infection can jeopardise implant success. Smoking—and, increasingly, vaping—are two such risk factors.
Smoking and Dental Implant Failure
Cigarette smoke contains thousands of harmful chemicals, including nicotine, carbon monoxide, and tar. These affect implant healing in several ways:
- Reduced blood flow: Nicotine causes blood vessels to constrict, limiting oxygen delivery to the tissues around the implant. This slows down osseointegration (Bain & Moy, 1993).
- Increased risk of infection: Smoking impairs immune function, making gum tissues more vulnerable to peri-implantitis, a destructive inflammation around implants (Heitz-Mayfield, 2008).
- Bone loss: Long-term smoking is linked to greater marginal bone loss around implants, compromising stability (Hinode et al., 2006).
Studies consistently show that implant failure rates are higher in smokers compared with non-smokers. For example, one review found that smokers are nearly twice as likely to experience implant failure (Chrcanovic et al., 2015).
What About Vaping?
Vaping is often marketed as a “safer” alternative to smoking. While e-cigarettes contain fewer carcinogens than tobacco, they still deliver nicotine and other substances that may affect implant healing.
- Nicotine in e-liquids: Just like smoking, vaping restricts blood flow to gum tissues. This can delay wound healing after implant surgery.
- Heat and chemicals: Vapourised propylene glycol and glycerine can cause dry mouth, reducing saliva’s protective effect against bacteria (Fraser et al., 2020).
- Inflammatory response: Emerging studies show vaping increases oxidative stress and inflammation in gum tissues, similar to smoking (Cichońska et al., 2019).
Although long-term research is limited, early evidence suggests vaping may still increase the risk of implant complications—though possibly to a lesser degree than smoking.
Peri-Implantitis: A Major Concern
One of the most significant complications related to smoking and vaping is peri-implantitis. This condition involves inflammation of the gums and bone around the implant, leading to progressive bone loss and potential implant failure.
Both smoking and vaping appear to increase susceptibility by altering the oral microbiome, reducing healing capacity, and impairing the body’s natural defence against bacteria (Heitz-Mayfield & Salvi, 2018). Once peri-implantitis develops, treatment becomes complex and outcomes are less predictable.
Improving Success Rates
If you are considering dental implants and you smoke or vape, it is important not to lose hope. Many patients in Worthing, Brighton, and across Sussex who smoke still benefit from implants—provided they take certain steps:
- Quit if possible: Stopping smoking (or vaping) before surgery significantly improves outcomes. Even short-term cessation of 1–2 weeks pre-surgery and up to 8 weeks post-surgery reduces complications (Clarke et al., 2012).
- Cut down gradually: If quitting altogether is difficult, reducing daily use can help improve blood flow and healing.
- Optimise oral hygiene: Regular brushing, flossing, and professional cleaning reduce bacterial load around implants.
- Attend maintenance visits: Implants require regular check-ups and hygiene visits to monitor gum health and prevent peri-implantitis.
- Consider nicotine replacement: Patches or gum may support healing better than smoking or vaping, as they avoid heat and toxic by-products.
Our Practice Approach
At the Clinic for Implant & Orthodontic Dentistry in Worthing, we take a personalised approach. Before recommending implants, we carefully review your medical history, smoking or vaping habits, and oral health status.
For patients who smoke or vape, we provide tailored advice on risk reduction, work closely with hygienists to support gum health, and offer regular monitoring after implant placement. With careful planning and maintenance, many patients still achieve excellent long-term outcomes.
Conclusion
Smoking and vaping both negatively impact dental implant success, mainly by reducing healing capacity and increasing the risk of peri-implantitis. While vaping may be less harmful than traditional smoking, it is not risk-free.
If you are considering implants, the best step you can take is to quit smoking or vaping entirely. If that is not possible, reducing use and committing to excellent oral hygiene and regular check-ups can still improve outcomes.
At our Worthing practice, we are here to help guide you through every step of your implant journey and support you in achieving a healthy, confident smile.
References
- Bain, C.A. & Moy, P.K. (1993). The association between the failure of dental implants and cigarette smoking. International Journal of Oral and Maxillofacial Implants, 8(6), 609–615.
- Chrcanovic, B.R., Albrektsson, T. & Wennerberg, A. (2015). Smoking and dental implants: A systematic review and meta-analysis. Journal of Dentistry, 43(5), 487–498.
- Cichońska, D. et al. (2019). The impact of e-cigarettes on oral health – a narrative review. Oral Health and Dental Management, 18(1), 1–8.
- Clarke, N.G. et al. (2012). Influence of smoking on oral wound healing: A review. Journal of Dental Research, 91(2), 119–123.
- Fraser, T., McCullough, M. & Gordon, C. (2020). E-cigarettes and oral health: A scoping review. Tobacco Induced Diseases, 18, 89.
- Heitz-Mayfield, L.J.A. (2008). Peri-implant diseases: Diagnosis and risk indicators. Journal of Clinical Periodontology, 35(Suppl 8), 292–304.
- Heitz-Mayfield, L.J.A. & Salvi, G.E. (2018). Peri-implant mucositis and peri-implantitis: A current understanding of their diagnoses and clinical implications. Journal of Periodontology, 89(Suppl 1), S257–S262.
- Hinode, D., Tanabe, S., Yokoyama, M. & Fujisawa, K. (2006). Influence of smoking on osseointegrated implant failure. International Journal of Oral and Maxillofacial Implants, 21(2), 294–299.
PMMA vs. Zirconia in All-on-4 Bridges: Why We Prefer PMMA for Full-Jaw Restorations - By Dr Amir Mostofi DDS, Dip. (Ortho.) , MSc (Implant.)
When selecting materials for All-on-4 implant bridges, our practice favours Poly(methyl methacrylate) (PMMA) over zirconia for full jaw restorations. This preference stems from PMMA's ability to be crafted with multiple layers, resulting in a more natural and lifelike appearance. Additionally, PMMA's lightweight nature offers enhanced comfort compared to the denser zirconia, which some patients may find heavier. Furthermore, PMMA bridges are easily repairable and more cost-effective, whereas zirconia bridges, though durable, can be challenging and expensive to fix if damaged. Therefore, PMMA presents a practical and aesthetically pleasing choice for patients seeking full jaw implant solutions.
When considering All-on-4 implant bridges—a dental procedure where a full arch of teeth is supported by four implants—it's essential to choose the right material for the prosthetic teeth. Two commonly used materials are poly(methyl methacrylate) (PMMA, a type of acrylic) and zirconia (a type of porcelain). At our practice, we have chosen to use PMMA for full jaw construction implant bridges. Here's why:
1. Aesthetics and Natural Appearance
High-quality PMMA teeth are typically crafted with multiple layers, allowing for a more natural and lifelike appearance. This layering technique enables dental technicians to mimic the translucency and shading variations found in natural teeth. In contrast, zirconia prosthetics are usually milled from a single layer, which can result in a more uniform and less natural look. Therefore, PMMA offers superior aesthetics, providing patients with a smile that closely resembles natural dentition.
2. Weight and Comfort
PMMA is a lightweight material, contributing to a more comfortable experience for patients. Zirconia, being denser, results in a heavier prosthesis. Some patients may find the additional weight of a zirconia bridge less comfortable, especially during the initial adjustment period. The lighter nature of PMMA can enhance overall comfort and adaptability. All On Four
3. Occlusal Considerations
When zirconia is used for both upper and lower bridges, patients may experience a clicking sound due to the contact between two hard surfaces, similar to the sound of porcelain teeth clashing. This phenomenon can be distracting and may affect the overall satisfaction with the prosthesis. PMMA, being a softer material, does not produce such noises, leading to a more natural and quiet biting experience. Dr. Sehmi
4. Repairability and Maintenance
One significant advantage of PMMA is its reparability. If a PMMA bridge chips or fractures, it can be easily and cost-effectively repaired without the need for extensive procedures. In contrast, zirconia bridges, while durable, are challenging to repair if damaged. A fracture in a zirconia prosthesis often necessitates the fabrication of an entirely new bridge, leading to increased costs and inconvenience for the patient.
5. Cost-Effectiveness
PMMA bridges are generally more affordable than their zirconia counterparts, making them an attractive option for patients seeking quality restorations without incurring high expenses. The lower cost does not compromise the aesthetic and functional outcomes, especially when considering the advanced layering techniques used in modern PMMA prosthetics.
Conclusion
While both PMMA and zirconia have their respective advantages, our practice has chosen to utilize PMMA for full jaw construction implant bridges due to its superior aesthetics, comfort, reparability, and cost-effectiveness. These factors align with our commitment to providing patients with natural-looking, durable, and affordable dental restorations.
For more information and a consultation visit, call us on 0190-821822 or visit our practice at 7 Chapel Road, Worthing BN111EG.
Closing the Gap: Effective Orthodontic Solutions for Gaps Between Upper Front Teeth (Midline Diastema) in Worthing, West Sussex - By Dr Amir Mostofi DDS, Dip. (Ortho.), MSc (Implant).
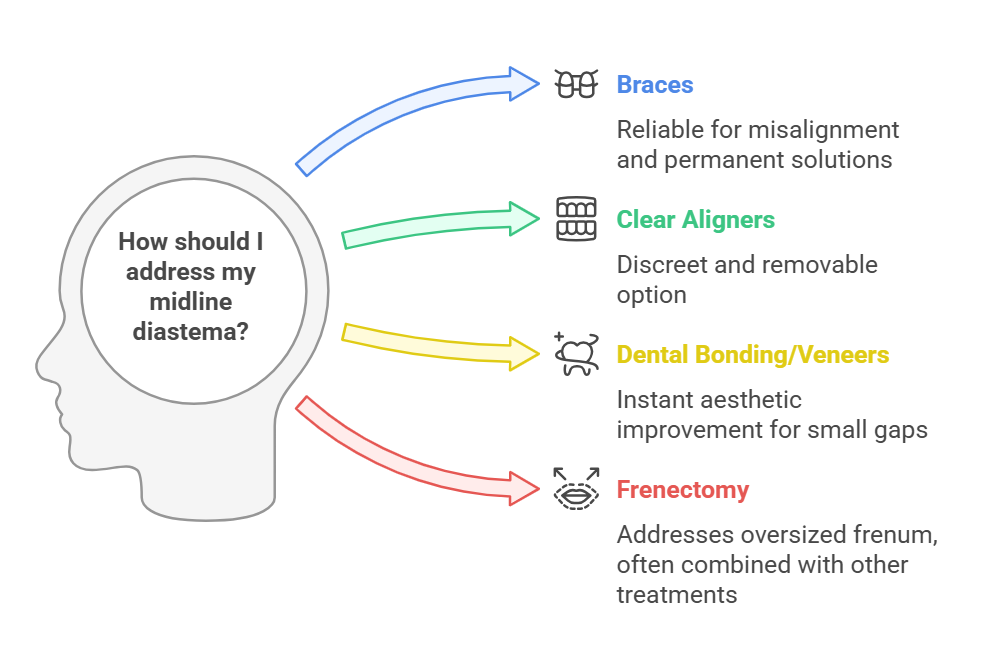
Do you have a gap between your upper front teeth (midline diastema) and wonder if orthodontic treatment can help? Many people feel self-conscious about this common dental issue, but modern orthodontic solutions can effectively close the gap and enhance both function and aesthetics. Whether you prefer braces, clear aligners, or cosmetic treatments like bonding or veneers, our expert team in Worthing, West Sussex, offers tailored solutions to meet your needs. Discover the causes of these gaps, treatment options, and how to maintain a beautifully aligned smile. Book your free consultation today and take the first step towards a confident new smile!
Are you self-conscious about the gap between your upper front teeth (midline diastema)? This common dental concern can affect both appearance and confidence. Fortunately, modern orthodontic treatments offer effective solutions to close this gap and give you a beautifully aligned smile. If you’re in Worthing, West Sussex, and looking for expert orthodontic care, our clinic is here to help.
What Causes Gaps Between Upper Front Teeth?
A gap between the upper front teeth (midline diastema) can occur due to various reasons, including:
- Genetics – If your family members have gaps in their teeth, you may inherit the same trait.
- Oversized Labial Frenum – The tissue connecting your upper lip to your gums may extend between your front teeth, preventing them from coming together.
- Mismatched Jaw and Tooth Size – When teeth are too small compared to the jawbone, spaces may appear between them.
- Habits and Oral Health Issues – Thumb sucking, tongue thrusting, or gum disease can contribute to the development of a gap between the teeth.
Why Should You Close the Gap?
While some people embrace their gap as a unique characteristic, others may feel self-conscious about it. Additionally, gaps between teeth can sometimes lead to oral health issues, including:
- Misalignment of Surrounding Teeth – Extra space can cause other teeth to shift, leading to bite problems.
- Difficulty Biting and Chewing – Gaps may affect how the teeth come together when eating.
- Increased Risk of Food Getting Stuck and Plaque Build-up – Gaps create extra spaces where food particles can get trapped, leading to a higher risk of cavities and gum disease.
- Speech Difficulties – Some people may develop a slight lisp due to improper tongue positioning.
Orthodontic Treatments to Close the Gap
At our Worthing-based orthodontic clinic, we provide customised treatment options to help close gaps between the upper front teeth (midline diastema) effectively:
1. Braces
Traditional metal braces or ceramic braces use gentle pressure over time to bring the teeth together. Braces remain one of the most reliable and permanent solutions for closing gaps between teeth. This method is especially effective for patients who have additional misalignment or bite issues.
2. Clear Aligners
For those looking for a more discreet treatment, Invisalign® clear aligners are an excellent alternative. These removable, nearly invisible trays gradually shift the teeth into alignment without the need for metal brackets or wires. Many patients in Worthing prefer Invisalign® because it allows them to maintain their confidence while undergoing treatment.
3. Dental Bonding or Veneers
For smaller gaps, cosmetic solutions like dental bonding or porcelain veneers may be an option. These treatments provide an instant aesthetic improvement but do not correct underlying alignment issues. Bonding is a quick and affordable option, while veneers offer a longer-lasting solution for those who want a flawless smile.
4. Frenectomy (If Necessary)
If an oversized labial frenum is the cause of your gap, a minor surgical procedure known as a frenectomy can help. This is often combined with orthodontic treatment to ensure long-term results. Without addressing the root cause, gaps may reopen even after orthodontic intervention.
How Long Does Treatment Take?
The duration of treatment depends on the method chosen and the severity of the gap:
- Braces – Typically, 6 to 12 months.
- Invisalign® – Around 6 to 12 months, depending on the case.
- Dental Bonding – Completed in a single appointment.
- Veneers – Requires two or more appointments.
- Frenectomy – A short procedure followed by healing time, after which orthodontic treatment may be needed.
Maintaining Your Results
After your treatment is complete, maintaining the results is crucial. Retainers are often recommended to prevent teeth from shifting back into their previous positions. Our Worthing orthodontists will provide you with a custom retainer and guidance on how to wear it effectively.
Why Choose Our Worthing Orthodontic Clinic?
Choosing the right orthodontic provider is essential for achieving the best results. Here’s why patients trust us:
- Expertise & Experience – Our team has years of experience in orthodontic treatments.
- State-of-the-Art Technology – We use the latest equipment to provide precise and effective treatments.
- Personalised Care – Each patient receives a tailored treatment plan to ensure the best possible outcome.
- Convenient Location in Worthing – Our clinic is easily accessible to residents in Worthing and the surrounding areas.
- Free Orthodontic Consultations – We offer complimentary consultations so you can explore your options without commitment.
Start Your Orthodontic Journey in Worthing
If you’re looking for professional orthodontic treatment in Worthing, West Sussex, our experienced team is ready to help you achieve a confident, gap-free smile. We offer free orthodontic consultations, allowing you to explore your treatment options and receive a personalised plan tailored to your needs.
Contact us today at Clinic for Implant & Orthodontic Dentistry in Worthing to schedule your appointment. Let’s transform your smile together!
📞 Call us at: 01903-821822
🌍 Visit our website: dental-worthing.co.uk
📍 Location: 7 Chapel Road, Worthing, West Sussex, BN11 1EG
Supporting Patients with Agoraphobia and Dental Anxiety: How We Can Help
Overcoming Dental Anxiety and Agoraphobia: Support for a Healthier Smile
Dental anxiety and agoraphobia can make maintaining oral health a daunting challenge, but you’re not alone. At the Clinic for Implant & Orthodontic Dentistry, we specialise in providing compassionate, home-based dental care for patients who struggle with anxiety or fear of leaving home. Our experienced team, led by Dr. Amir Mostofi, offers a full range of services—from examinations and X-rays to fillings and extractions—all in the comfort of your home. Discover how we can help break the cycle of dental anxiety and support your journey to better oral health.
Read the full article to learn more about our services and how we can help you feel at ease.
Dental anxiety, often referred to as fear, anxiety, or stress associated with a dental setting, can pose significant challenges to maintaining oral health. For individuals with conditions like agoraphobia—a fear of being in situations where escape may feel difficult—accessing dental care can feel overwhelming. At the Clinic for Implant & Orthodontic Dentistry, we understand these challenges and are here to help.
Understanding Dental Anxiety and Its Causes Dental anxiety can be triggered by various factors, such as the fear of needles, drills, or the overall dental environment. In its severe form, dental anxiety becomes a phobia, leading to avoidance of dental care. This avoidance can result in a cycle of worsening oral health, which may further heighten anxiety.
Conditions such as generalised anxiety disorder, post-traumatic stress disorder (PTSD), depression, or previous trauma to the head and neck can increase susceptibility to dental anxiety. Additional triggers might include a perceived invasion of personal space, fear of losing control, or trust issues. Agoraphobia, in particular, can exacerbate dental anxiety, as the idea of attending a dental clinic may feel insurmountable.
The Importance of Regular Dental Care Avoiding dental visits due to anxiety or agoraphobia can lead to preventable oral health problems such as gum disease, tooth decay, and even more serious conditions like oral cancer. Routine dental check-ups allow early detection of issues, enabling simpler and less invasive treatments. Good oral hygiene is also essential for overall health, as oral diseases are linked to conditions like diabetes, heart disease, and stroke.
Maintaining oral health starts with regular brushing, flossing, and professional cleanings. For those struggling with dental anxiety, ensuring consistent dental visits is critical to breaking the cycle of avoidance and anxiety.
How We Help Patients with Agoraphobia and Anxiety Our practice specialises in supporting patients with dental anxiety and agoraphobia, offering a compassionate and tailored approach. Dr. Amir Mostofi, our principal dentist, has over 20 years of experience working with anxious and agoraphobic patients. We provide a domiciliary dental service, visiting patients in the comfort of their homes across Sussex, Surrey, London, Bristol, and Suffolk.
Services we offer include:
- Full dental examinations
- X-rays
- Fillings
- Crowns
- Dentures
- Extractions
Our team takes the time to understand each patient's unique needs and anxieties. By creating a calm and stress-free environment, we help patients feel at ease during their appointments. Additionally, we offer options for sedation and relaxation techniques, including happy gas (nitrous oxide), oral anxiety-relieving medications, and conscious sedation, ensuring treatments are as comfortable as possible.
Breaking the Cycle of Dental Anxiety Open communication is key to managing dental anxiety. We encourage patients to share their concerns, enabling us to create a personalised care plan. Techniques such as deep breathing, listening to music, or agreeing on a stop signal during treatment can also make a significant difference.
For those unable to visit a traditional dental clinic, our mobile dental service ensures that essential care is accessible. By addressing dental issues in a familiar environment, we aim to build trust and confidence, empowering patients to take charge of their oral health.
Let Us Support You At the Clinic for Implant & Orthodontic Dentistry, we are committed to helping patients with agoraphobia and dental anxiety maintain their oral health. If you or a loved one struggles with visiting the dentist, contact us today. Together, we can break the cycle of anxiety and ensure a healthier, happier smile.
Your oral health matters, and we’re here to help every step of the way.
The Importance of Routine Dental Check-ups - By Bo Conley
The Importance of Routine Dental Check-ups
Regular dental check-ups are essential for maintaining healthy teeth and gums. At the Clinic for Implant & Orthodontic Dentistry in Worthing, we recommend visiting your dentist every six months to prevent issues like tooth decay and gum disease. Routine check-ups include professional cleanings and early detection of dental problems, helping to avoid costly treatments later. Whether you're in Worthing, Brighton and Hove, Sussex, Surrey, or London, our practice offers flexible appointments, emergency services, and mobile dental care for your convenience. Keep your smile healthy by booking your next check-up today! Call us on 01903 821 822, Worthing, West Sussex.
The Importance of Routine Dental Check-ups
Maintaining good oral health is essential for overall well-being, and regular dental check-ups are a crucial part of this process. Whether you are in Worthing, Brighton and Hove, Sussex, Surrey, or London, visiting your dentist routinely can prevent serious dental issues and ensure your teeth and gums remain healthy.
At the Clinic for Implant & Orthodontic Dentistry in Worthing, we strongly recommend that patients attend dental check-ups every six months. These appointments allow your dentist to thoroughly assess your oral health and identify any potential problems early on. By doing so, you can avoid more complex treatments down the line, which may be more costly and invasive.
Prevention is Better Than Cure
The primary benefit of routine dental check-ups is prevention. During these visits, your dentist will examine your teeth and gums for signs of decay, gum disease, and other dental issues. Early detection of problems such as cavities, gingivitis, or worn-down enamel can prevent them from developing into more severe conditions.
For patients in Brighton and Hove or Sussex, who may have busy schedules, our clinic offers flexible appointment times. We also provide advice on how to maintain good oral hygiene between visits, ensuring that you have the knowledge and tools to protect your teeth and gums at home.
Professional Cleaning
A regular dental check-up also includes a professional cleaning session. While daily brushing and flossing are vital for maintaining oral health, a dentist or hygienist can reach areas that are often missed. Plaque and tartar build-up can lead to tooth decay and gum disease if not removed regularly. Professional cleaning during your check-up helps to remove these deposits, keeping your mouth healthy and fresh.
Whether you are in Sussex or Surrey, regular cleanings are a key component of preventing more serious issues such as periodontitis, a severe form of gum disease that can lead to tooth loss.
Detecting Early Signs of Health Conditions
Routine dental check-ups also play an essential role in the early detection of other health conditions. Dentists can identify signs of oral cancer, diabetes, and even heart disease during a thorough examination. Early detection significantly improves treatment outcomes, making regular dental visits critical to your overall health.
Emergency Dental Care and Mobile Dental Services
While routine check-ups are vital for prevention, dental emergencies can still occur. Our practice in Worthing offers emergency dental services, ensuring that if you experience severe tooth pain, a broken tooth, or another urgent dental issue, you can receive prompt and effective treatment.
For those who are unable to visit the clinic in person, we also offer mobile dental services across Sussex, Surrey, and London. Our mobile dentist team brings quality dental care to your doorstep, ensuring that even those with mobility issues can receive the check-ups and treatments they need.
Conclusion
Regular dental check-ups are vital for maintaining oral health and preventing future complications. Whether you're based in Worthing, Brighton and Hove, Sussex, Surrey, or London, attending these routine appointments will help ensure your teeth and gums remain in the best possible condition. At the Clinic for Implant & Orthodontic Dentistry, we provide comprehensive dental care, including emergency services and mobile dental services, to meet the needs of all our patients. Book your next check-up today and take the first step toward a healthier smile.
Lost Dentures During a Patient's Hospital Stay: A Common Problem and How We Can Help
Losing dentures during a hospital stay is a common yet distressing issue that can significantly impact a patient's comfort and ability to eat properly. At the Clinic for Implant & Orthodontic Dentistry in Worthing, we offer a convenient mobile dental service to replace lost dentures, providing custom-made solutions directly in the hospital. Whether you're in Sussex, Surrey, or London, our team is ready to assist, ensuring you regain your comfort and dignity quickly. Learn how we can help and the steps hospital staff can take to prevent this issue.
Lost Dentures in NHS Hospitals? Private Mobile Dental Service in Worthing, Sussex, Surrey, and London
Losing dentures during a hospital stay is an increasingly common issue that can cause significant distress for patients. Whether it's due to a short stay for a routine procedure or a longer stay for more serious health concerns, misplaced or lost dentures can severely impact a patient's ability to eat properly, chew, and maintain their overall comfort. Unfortunately, this issue is all too familiar within hospitals across Worthing, Sussex, Surrey, and London.
Hospitals are busy environments where patients are often moved between wards, and their personal belongings, including dentures, can easily become misplaced. This can occur due to a variety of reasons, such as being moved to a different bed, confusion among hospital staff, or simply being misplaced by the patient themselves, particularly if they are unwell or disoriented. The impact of lost dentures can be profound, leading to difficulty in eating, discomfort, and even embarrassment, especially if the patient is in the hospital for an extended period.
For patients, the loss of dentures is more than just an inconvenience; it is a significant healthcare issue. Without dentures, patients may struggle with chewing, leading to nutritional challenges and discomfort. This problem can be particularly acute for elderly patients, who are more likely to be admitted for long-term care. It’s crucial for hospital staff, including nurses and healthcare assistants, to be aware of the importance of dentures and take extra care to prevent them from being lost.
At the Clinic for Implant & Orthodontic Dentistry in Worthing, we understand the distress that lost dentures can cause. That’s why we offer a comprehensive mobile dental service, also known as a domiciliary dental service, to assist patients who have lost their dentures during a hospital stay. Our team of experienced dentists can visit patients directly in the hospital, whether in Worthing, Sussex, Surrey, or London, to provide immediate assistance.
Our mobile dental service is designed to be convenient and efficient, ensuring that patients who have lost their dentures can quickly get a replacement. We offer a range of denture options, including fully acrylic dentures and cobalt chrome dentures for both upper and lower teeth. These high-quality dentures are custom-made to fit each patient’s needs, allowing them to regain their ability to eat, chew, and speak comfortably.
For patients staying in NHS hospitals, we provide detailed information on the costs associated with replacement dentures and offer support in navigating the process to ensure they receive the care they need. As a private practice, our service is particularly beneficial for patients who may not be able to visit a dental practice due to their hospital stay or health condition.
In addition to providing new dentures, we also work closely with hospital staff to raise awareness about the importance of denture care during a patient’s stay. By educating nurses, healthcare assistants, and other hospital staff about the risks of lost dentures and the steps that can be taken to prevent this issue, we aim to reduce the frequency of this common problem.
In summary, lost dentures during a hospital stay are a significant issue that can impact a patient's health and wellbeing. At the Clinic for Implant & Orthodontic Dentistry, we are committed to providing prompt and effective solutions through our mobile dental service, ensuring that patients can quickly regain their comfort and dignity. If you or a loved one has lost dentures during a hospital stay, please contact us for assistance. Our team is here to help, providing the care and support needed to restore your smile.
Ensuring Your Safety with Our Astringent Sterilisation Processes - by Bo Conley
At the Clinic for Implant & Orthodontic Dentistry in Worthing, West Sussex, patient safety is our top priority. We offer comprehensive dental services, including emergency appointments, dental implants, fillings, and braces. Our rigorous sterilisation processes ensure a hygienic environment, whether you're visiting from Worthing, Lancing, Goring-by-Sea, Brighton, or Shoreham-by-Sea. Our skilled orthodontists and dental nurses uphold the highest standards of cleanliness, using advanced autoclave technology and hospital-grade disinfectants. We are dedicated to providing the best care in the safest environment for all our patients.
At the Clinic for Implant & Orthodontic Dentistry in Worthing, West Sussex, patient safety is always our top priority. We are dedicated to providing excellent dental care, and this commitment is reflected in our meticulous and astringent sterilisation processes. Whether you are visiting us for a routine check-up, an emergency appointment, or specific treatments like root canals, crowns, bridges, dentures, or teeth whitening, you can rest assured that every precaution has been taken to ensure a safe and hygienic environment.
Sterilisation: The Cornerstone of Dental Safety Sterilisation in dentistry is the most important process of the protocols carried out in a clinic. It is crucial to pay attention to this procedure, as poor practices can lead to the spread of germs. At our clinic, we understand this responsibility and our staff always go above and beyond to ensure that the highest standard of sterilisation is maintained. We use the gold standard of sterilisation with our washer disinfector. By thoroughly cleaning your instruments using washer disinfectors, we subject the utensils to high heat for a prolonged period. This process effectively kills off bacteria, protecting both our patients and our staff.
Our Sterilisation and Disinfectant Procedures We understand that dental visits can sometimes be a source of anxiety, particularly when it comes to concerns about cleanliness and infection control. To address these concerns, we have implemented a rigorous sterilisation protocol that surpasses standard practices. Each of our dental instruments is thoroughly cleaned, disinfected, and sterilised using advanced autoclave technology. This high-pressure steam sterilisation process effectively eliminates all bacteria, viruses, and fungi, ensuring that every instrument is perfectly safe for use. In addition to instrument sterilisation, our dental chairs, surfaces, and workspaces are meticulously disinfected after each patient visit. We use hospital-grade disinfectants known for their efficacy in killing a broad spectrum of pathogens. This comprehensive approach helps to maintain a sterile environment at all times.
Caring and Thorough Dental Nurses Our team of highly trained dental nurses plays a crucial role in maintaining our high standards of cleanliness and patient care. They take the time to ensure that every procedure is performed with the utmost precision and care. From setting up the treatment rooms to assisting during procedures, our nurses are diligent in their efforts to uphold our stringent sterilisation protocols.
Emergency Dental Visits We understand that dental emergencies can occur unexpectedly and require immediate attention. In such cases, our clinic is equipped to provide prompt and effective care. During emergency appointments, our primary concern is to alleviate pain and address the immediate problem. Even in emergency situations, we do not compromise on our sterilisation and safety standards. Every effort is made to ensure that our emergency services are delivered in a safe and controlled environment.
Comprehensive Dental Services Beyond emergency care, we offer a wide range of dental services, including root canals, crowns, bridges, dentures, and teeth whitening. Each of these treatments is carried out with the same level of attention to sterilisation and patient safety. For instance, during a root canal procedure, every instrument and material used is sterilised to prevent any risk of infection. Similarly, for treatments like teeth whitening, we ensure that all tools and products are prepared in a sterile environment to guarantee the best results without compromising safety.
Commitment to Patient Safety Our commitment to patient safety is unwavering. From routine check-ups to complex dental procedures, we adhere to the highest standards of sterilisation and disinfection. This commitment is integral to our practice and is a testament to the trust our patients place in us. At the Clinic for Implant & Orthodontic Dentistry, we believe that every patient deserves the best care in the safest environment. We are proud to serve the Worthing community and are dedicated to maintaining the health and well-being of all our patients through our stringent sterilisation processes and comprehensive dental care services. For more information or to schedule an appointment, please visit our website at dental-worthing.co.uk or call us at 01903-821822. Your safety and satisfaction are our top priorities.
Dental implants in patients affected by systemic diseases - By Dr Amir Mostofi -DDS, Dip. (Ortho.), MSc(Implant.)
Navigating the intricate landscape of dental implantology amidst systemic diseases demands a nuanced understanding and approach. The comprehensive review by Donos and Calciolari delves deep into how systemic health conditions and their associated medications influence the success of dental implants. It highlights the paramount importance of meticulous patient selection, informed by a thorough medical history and the complexity of the surgical site. This narrative is not just about the challenges; it offers a beacon of guidance with practical suggestions for clinicians, aiming to mitigate risks and optimise outcomes. It also casts a spotlight on the need for further research to refine our understanding of these interactions. This exploration serves as a crucial resource for dental professionals, ensuring they are well-equipped to provide care that combines the dual goals of patient safety and implant success.
Dental implants in patients affected by systemic diseases
The exploration of dental implant success among patients burdened by systemic diseases reveals a realm of nuanced considerations, pivotal for optimising patient care and outcomes. Authored by N. Donos and E. Calciolari and published in the British Dental Journal in 2014, this comprehensive review sheds light on the intersection between systemic health conditions and dental implantology, presenting an invaluable resource for dental professionals worldwide.
Systemic diseases, encompassing a wide array of health conditions, often necessitate medications that could influence or complicate the process of dental implant surgery. Understanding the intricate relationship between these systemic conditions and dental implant success is crucial for clinicians, as it aids in the meticulous planning and execution of implant surgeries, ensuring both the safety and well-being of patients. This narrative delves into the evidence surrounding implant survival and success in patients with systemic diseases, offering practical suggestions for clinicians and highlighting areas necessitating further research.
Dental implants represent a cornerstone in the treatment of edentulism, showcasing high survival rates and offering a semblance of natural dentition. The essence of achieving successful implant outcomes lies in judicious patient selection, entailing a thorough medical history evaluation and a comprehensive assessment of the surgical site's complexity. Certain systemic conditions, underscored by varying levels of evidence, have been identified as potential complicating factors or even contraindications to implant surgery. This increasing prevalence of medically compromised individuals seeking dental implants underscores the importance of understanding the impact of systemic diseases and associated medications on both the surgical procedure and the overall treatment outcome.
Among the systemic conditions deemed as absolute contraindications for implant surgery are recent cardiovascular events, recent major surgeries such as valvular prosthesis placement or organ transplants, heightened risk of bleeding, significant immunosuppression, active cancer treatment, and intravenous bisphosphonate therapy. These conditions pose not only a heightened risk of implant failure but also potential grave risks to the patient's overall health.
The review further explores the effect of various systemic diseases on dental implant outcomes, with a focus on bone diseases such as osteoporosis, medication-related osteonecrosis of the jaws (MRONJ), and other less common bone conditions. Osteoporosis, a prevalent bone disease, poses biological plausibility for impaired bone healing around implants, though evidence remains controversial. Antiresorptive medications, particularly bisphosphonates and denosumab, present a risk for MRONJ, influencing implant success rates and necessitating careful patient management.
Diabetes mellitus, characterised by hyperglycemia, has been shown to negatively impact bone metabolism and may impede osseointegration and implant success. The review emphasises the importance of glycaemic control in diabetic patients undergoing implant therapy, alongside the management of other complications associated with diabetes.
Cardiovascular diseases, bleeding disorders, and specific mucosal diseases such as oral lichen planus and ectodermal dysplasia are also scrutinized for their potential impact on dental implant outcomes. The review suggests tailored approaches and precautionary measures for patients with these conditions, aiming to maximise implant success while minimising risks.
The document culminates in general clinical recommendations, underscoring the limited evidence base concerning the effect of systemic diseases on dental implant success. It calls for larger prospective studies to enhance understanding and provide more definitive guidance. Despite a few conditions being labelled as absolute contraindications, the review advises dental professionals to weigh the benefits and risks of implant therapy carefully, engage in interdisciplinary communication, and adopt stringent follow-up regimens for patients with systemic diseases.
In essence, the review by Donos and Calciolari serves as a testament to the complexity of dental implantology within the context of systemic health. It beckons a holistic approach to patient care, emphasising the need for ongoing research, clinical prudence, and a deep understanding of the interplay between systemic diseases and dental implant outcomes.
The Journey of 'All on 4' Dental Implants - A Poetic Insight
In the realm of dental marvels, the 'All on 4' procedure stands as a beacon of hope for those yearning for a permanent solution to their dental woes. Through the lens of poetry, we embark on a poignant journey from apprehension to elation, as patients traverse the path of transformation. This piece eloquently captures the essence of overcoming fears, enduring temporary discomfort, and the financial considerations involved in the pursuit of a flawless smile. It serves as a testament to the power of resilience and the artistry of dental innovation, ultimately revealing the joy and confidence that come with a renewed smile.
The Journey of 'All on 4' Dental Implants - A Poetic Insight
In the heart of dental innovation's stride,
Lies a journey, profound and wide,
-------
"All on 4," a beacon of hope,
For those at the end of their tether's rope.
-------
From dentures that shift, to gaps that dismay,
Patients seek a brighter, steadfast way.
------
Gone are the teeth, in both jaws, they part,
Making room for a new, enduring start.
-------
Four to six pillars, implanted deep,
Promising a smile, once more to keep.
-------
A bridge, permanent, fixed and true,
A transformative path, for the chosen few.
-------
Yet, fear shadows the steps to be made,
The unknown, a daunting, lurking shade.
-------
Discomfort, a guest, in the weeks to ensue,
A price, not just monetary, paid by the few.
-------
The venture's costly, a truth well known,
Some seek abroad, into the unknown.
-------
Yet wisdom speaks, in choosing with care,
An established dentist, with skill rare.
-------
Interest-free solutions, to ease the expense,
A gesture, making the decision less tense.
-------
Initial consults, x-rays to guide,
A plan unfolds, with the expert by your side.
-------
For those with nerves, frayed and worn,
Sedation offers, a calm before the morn.
-------
Patience, a virtue, as time unfolds the tale,
Of transformation, where once confidence did pale.
-------
Through hurdles and challenges, the journey is long,
But in perseverance, one finds they're strong.
-------
A smile, once hidden, now brilliantly beams,
Reflecting a journey, of hopes and dreams.
-------
"All on 4," more than a procedure, a start,
To reclaiming joy, with dental art.
-------
From hesitant steps to a confident smile,
A testament to courage, mile after mile.
Understanding Dental Bone Grafts: A Comprehensive Guide - By Dr Amir Mostofi DDS , Dip (Ortho.), MSc (Implant.)
Dental bone grafts are essential procedures for restoring jawbone structure and are crucial for dental implants and overall oral health. They involve adding bone material to the jaw, aiding in bone regeneration, and providing a stable foundation for future dental work.
Understanding Dental Bone Grafts: A Comprehensive Guide
Dental bone grafting is a crucial procedure for patients experiencing jawbone loss, which can significantly impact oral health and the success of dental implants. It involves adding bone material to the jaw, which can be sourced from various origins such as the patient's own body, human or animal tissue banks, or synthetic materials. This procedure acts as a scaffold, allowing the patient's own bone tissue to grow and regenerate. Dental bone grafts are often essential for individuals who have lost teeth, are planning dental implant surgery, require dentures, or have suffered bone loss due to gum disease.
Types of Dental Bone Grafts
There are several types of dental bone grafts, each serving a unique purpose:
Socket Preservation: Performed immediately after tooth extraction to prevent socket collapse.
Ridge Augmentation: Enhances the jawbone's width and volume, particularly after long-term tooth loss.
Sinus Lift: Elevates the maxillary sinuses to allow for implant placement in the upper jaw.
Periodontal Bone Graft: Targets bone loss caused by gum disease, providing stability to loose teeth.
Procedure Details
Before the Procedure The process begins with a thorough oral examination and dental imaging to assess bone loss. Based on these findings, a personalized treatment plan is developed.
During the Procedure The procedure involves administering local anesthesia, making a small incision in the gums, and placing the bone graft material in the required area. A membrane may cover the graft for added protection. Finally, the incision is closed with stitches.
After the Procedure Post-surgery, patients might experience pain, swelling, and bruising, which are manageable with pain relievers and possibly antibiotics. It's normal to find small bone fragments in the surgical area during initial healing.
Pain and Sedation Dental bone grafts are generally low in pain. Sedation options vary, from local anesthesia to general anesthesia, depending on the case complexity.
Success and Failure The success rate of dental bone grafts is high, but smoking or certain medical conditions can increase the risk of failure. Warning signs include worsening pain, pus, gum recession, and lack of jawbone improvement.
Risks and Benefits
While generally safe, potential risks include infection, bleeding, nerve damage, and anesthesia complications. The benefits include increased eligibility for dental implants and restoration of jaw structure.
Recovery and Outlook
Recovery varies, typically taking three to nine months for complete healing. Most people can resume normal activities the day after surgery.
When to Contact Healthcare Providers
Patients should watch for severe pain, increased swelling, pus around the grafting site, or fever and contact their dentist if these occur.
Summary
Dental bone grafts are vital for restoring oral health and function in individuals with jawbone loss. They play a critical role in preparing for dental implants and combating the effects of tooth loss and gum disease.
Navigating the Misconceptions: Bone Grafting and All on 4 Dental Implants- By Dr Amir Mostofi DDS, Dip. MSc
The All on 4 dental implant technique is transforming full jaw restoration, challenging long-held beliefs about bone grafting. Traditionally, dental implants often required bone grafting to compensate for insufficient bone volume. However, All on 4 implants frequently bypass this necessity due to their unique design and placement strategy. This innovative method involves positioning four implants in the jaw, utilizing existing bone structure, even where volume is limited. The success of this procedure, especially without bone grafting, heavily relies on the dentist's skill and precision. Experienced professionals adept in implantology can effectively leverage the jaw's anatomy, reducing the need for additional invasive procedures. Avoiding bone grafting offers numerous advantages, including shorter treatment times, less invasive surgery, and faster recovery. This approach not only enhances patient comfort but also immediately improves dental functionality and aesthetics.
Navigating the Misconceptions: Bone Grafting and All on 4 Dental Implants.
By Dr Amir Mostofi DDS, Dip. MSc
The realm of dental implant technology has witnessed significant advancements in recent years, with All on 4 dental implants emerging as a pivotal solution for full jaw rehabilitation. This revolutionary technique has not only enhanced the efficiency of dental restorations but has also challenged common perceptions, particularly regarding the necessity of bone grafting.
Understanding All on 4 Dental Implants:
All on 4 dental implants offer a comprehensive solution for patients with significant tooth loss. This procedure involves the strategic placement of four implants in the upper or lower jaw, providing a stable foundation for a full-arch prosthesis. The technique is celebrated for its minimally invasive nature and its ability to deliver immediate results.
Debunking Bone Grafting Myths in All on 4 Implants:
Contrary to popular belief, All on 4 dental implants often do not require bone grafting. This misconception stems from traditional implant procedures where insufficient bone volume necessitated grafting. However, the innovative design and strategic placement of All on 4 implants typically bypass the need for such additional procedures.
The Science Behind No-Bone-Grafting in All on 4 Implants:
The key lies in the angulation and placement of the implants. By tilting the posterior implants, All on 4 takes advantage of the existing bone structure, even in cases where bone volume is limited, thereby eliminating the need for grafting in many instances.
Expertise Matters: The Role of Skilled Dental Professionals:
The success of All on 4 implants without bone grafting hinges on the expertise of the dental professional. Precision in implant placement is crucial, requiring an in-depth understanding of oral anatomy and advanced surgical skills. This expertise ensures optimal use of available bone and minimizes the need for grafting.
Advantages of Avoiding Bone Grafting:
Avoiding bone grafting in All on 4 procedures offers several benefits:
Reduced treatment time
Less invasive surgery
Lower risk of complications
Quicker recovery and healing
Immediate improvement in functionality and aesthetics
Conclusion
All on 4 dental implants represent a significant leap forward in oral rehabilitation. By potentially eliminating the need for bone grafting, they offer a quicker, less invasive, and more efficient solution for full jaw restoration. However, the key to success lies in the hands of skilled dental professionals whose expertise can make a significant difference in the outcome. As with any medical procedure, it's essential for patients to consult with experienced dental practitioners to explore the best options for their specific needs.
Choosing Denplan: Affordable Dental Care for Worthing residences
Are you searching for accessible, high-quality dental care in Worthing, United Kingdom? Look no further than the Clinic for Implant & Orthodontic Dentistry. Our Denplan offers an array of benefits, including free routine check-ups, dental hygiene, fillings, root canals, extractions, and emergency treatments. Plus, for treatments involving laboratory work, patients only cover the lab fee. Denplan also includes worldwide emergency dental coverage. While it doesn't cover orthodontics, implants, or cosmetics, our clinic goes the extra mile, offering Denplan patients a 20% discount on these treatments. Join Denplan today for budget-friendly, top-notch dental care.
Are you seeking an affordable way to maintain your oral health without breaking the bank? Look no further! At the Clinic for Implant & Orthodontic Dentistry in Worthing, we understand the importance of good-quality dentistry, and we're dedicated to making it accessible to everyone. That's why we offer Denplan, an excellent dental maintenance plan that provides comprehensive coverage and benefits to our valued patients. In this blog, we'll explore what Denplan is, how it works, and why it's an excellent choice for those in search of budget-friendly dental care.
Denplan: Your Gateway to Quality Dental Care
At our practice, we believe that good-quality dentistry, the expertise of a well-trained dentist, and top-notch dental materials shouldn't come at a hefty price. To ensure our patients are shielded from the rising costs of dental treatments, we've introduced Denplan, a comprehensive dental maintenance plan that offers a range of benefits, including:
Free Routine Dental Check-Ups: Regular check-ups are crucial for maintaining your oral health. With Denplan, you'll have access to free routine dental check-ups, ensuring your dental needs are regularly assessed.
Dental Hygiene: Keeping your teeth clean and healthy is essential. Denplan covers dental hygiene treatments, helping you maintain a bright and healthy smile.
Fillings and Root Canal: Should you require fillings or root canal treatments, Denplan has you covered, reducing the financial burden of these essential procedures.
Extractions and Emergency Treatments: Dental emergencies can happen unexpectedly. Denplan provides coverage for extractions and emergency treatments, giving you peace of mind.
Laboratory Work: For treatments involving laboratory work, such as dentures, crowns, bridges, and post and core procedures, Denplan patients only pay the lab fee, typically around 10%–15% of the treatment cost.
Worldwide Emergency Dental Cover: Whether you're at home or abroad, Denplan offers worldwide emergency dental cover, ensuring you're protected no matter where you are.
It's important to note that while Denplan is comprehensive, it does not cover orthodontic treatments (braces), purely cosmetic treatments, or dental implants. Denplan is designed as a dental maintenance plan and is best suited for those without immediate outstanding treatment needs.
But here's the exciting part: even though Denplan doesn't cover orthodontics, implants, or cosmetics, our practice goes the extra mile. We offer Denplan patients a generous 20% discount on these treatments, making quality dental care even more accessible.
Denplan Care: A Closer Look
Denplan Care, provided by Denplan (Simply Health), is an affordable monthly payment scheme that allows you to budget for your routine dental care and treatment. This comprehensive plan covers a wide range of services, including:
Inspections and X-rays
Dental Hygiene Visits, Preventive Dental Advice
Gum Treatment
Fillings
Root Canal Treatment
Crowns, Bridges, and Dentures (excluding laboratory fees) The only exclusions are prescriptions, referrals to specialists or specialist treatments, orthodontics, implants, and cosmetic treatments. As part of your dental plan, Denplan also arranges supplementary insurance to cover eligible dental treatment resulting from dental injuries and emergencies in the UK or abroad.
With over 6,500 dentists across the UK looking after 1.8 million patients under Denplan Care, you can trust that you're in good hands. The primary focus of Denplan Care is on providing quality, preventive care, helping you maintain your oral health effectively.
Monthly Fees Tailored to You
Denplan monthly fees are determined by your dentist based on your oral health and anticipated future treatments. These fees also take into account the unique operating costs of your dental practice, which can vary from one practice to another. This personalized approach ensures that you pay a fair and reasonable monthly fee that aligns with your specific dental needs.
In conclusion, Denplan is your ticket to quality dental care without the financial strain. While many dental practices don't cover implant, cosmetic, or orthodontic treatments under Denplan, we stand out by offering a generous 20% rebate to Denplan patients for these treatments.
For more detailed information about Denplan or to request a brochure, please feel free to pop into our clinic at 7 Chapel Road, Worthing, West Sussex BN11 1EG, or give us a call at 01903-821822. We're here to provide you with the best dental care Worthing has to offer, all within your budget.
Choose Denplan today and enjoy a lifetime of healthy smiles!
Creating Perfect Dentures at Home with a Dentist Who Comes to You- By Dr Amir Mostofi DDS Dip MSc
Creating custom dentures at home with the expertise of a domiciliary dentist is an ideal solution, especially for patients facing unique challenges. Clinic for Implant & Orthodontic Dentistry prioritises patient-centred care, ensuring the utmost comfort and satisfaction throughout the process. Our journey begins with a comprehensive initial consultation, followed by extractions if necessary. Accurate impressions of your jaw are taken, even in cases of shrinking jawbones. We provide flexibility, allowing alterations during the wax trial denture stage at no extra cost. For those with cobalt chrome dentures, we handle the challenges seamlessly. We also offer domiciliary dental care for home-bound or bed-bound patients, ensuring safety and convenience. Our goal is to craft dentures that restore your smile and improve your quality of life.
Creating Perfect Dentures at Home with a Dentist Who Comes to You
Dentures made in the convenience of one's own home with the assistance of a domiciliary dentist are an excellent option for those who find traditional dental visits difficult. At Clinic for Implant & Orthodontic Dentistry, we specialise in providing denture services that are tailored to the specific requirements of our patients, including those with dementia and other mental disorders. In this exhaustive guide, we will walk you through the various phases of denture creation, from initial consultations to the final fitting, while emphasising the significance of a domiciliary dentist's experience in managing complex cases.
Step 1: Consultations at the outset
The initial consultation is a crucial first stage in the process of acquiring dentures. During this appointment, our domiciliary dentist conducts a comprehensive examination of your oral health and discusses the denture options that best meet your requirements. For a number of our patients, particularly those with dementia, collecting impressions can be difficult. Our experienced domiciliary dentists play a crucial role in the management of such cases. During this phase, we also ensure that all necessary documentation, including consent forms and cost discussions, is completed.
Step 2: Extraction, if Required
When oral health issues are identified during the initial consultation, tooth extraction may be required. To minimise patient distress, tooth extraction is performed with care and frequently in stages. This period, which typically lasts between one and three weeks, allows the mouth to recuperate and reduces swelling, making future dentures fit better.
Step 3: Taking Impressions
Taking accurate impressions of your upper and lower mandible is a crucial step in the fabrication of dentures that fit securely and comfortably. Numerous elderly individuals struggle with thinning jawbones, necessitating the use of specialised impression-taking techniques. Our domiciliary dentists are well-versed in adapting these techniques to individual requirements, thereby ensuring an accurate representation of your mandible and any remaining teeth.
Step 4: Registration of the Bite
At the stage of bite registration, the complex relationship between your upper and lower mandible is established. This procedure enables the dentist to record the precise relationship between your jaws. In addition, during this phase, the colour, shape, size, and quality of the denture teeth are meticulously determined, ensuring that your dentures appear and feel natural.
Step 5: Wax trial dentures
Seeing the wax trial dentures in your mouth is a crucial step in the process of creating dentures. This phase enables both you and the dental technician to evaluate whether the desired aesthetic has been achieved. At this juncture, any necessary modifications can be discussed and implemented. At Clinic for Implant & Orthodontic Dentistry, we prioritise your satisfaction, and alterations are made at no additional cost if necessary.
Step 6: Final Fitting and Adjustments
In the final stage, the completed dentures are adjusted. If significant changes were made during the wax trial denture stage, it may be necessary to repeat appointment 4. We recognise that the process of having dentures fitted can be intimidating, especially for first-timers or those who have had negative experiences in the past. Our dedication to ensuring that you comprehend the procedure and our emphasis on both form and function ensure that you leave with dentures that inspire confidence.
Visits and Problems with Cobalt Chrome Dentures
Generally, between four and seven visits are required to complete a denture, depending on the individual's requirements and complexity. However, cobalt chromium dentures, which contain a metal skeleton, typically require more visits due to the complexity of their fabrication and adjustment. Our skilled team at Clinic for Implant & Orthodontic Dentistry is well-equipped to handle such challenges, assuring the best possible outcome for your cobalt chrome dentures.
Domiciliary dental care for patients confined to their homes or beds
We recognise that not all patients have easy access to dental clinics. For this reason, we offer home visits, also known as domiciliary dental care, to those who are bedridden or confined to their homes. We make the process as convenient and comfortable as possible for patients who can recline in a wheelchair or regular chair with space around the dentist's workspace.
If a patient is completely bedridden and inclining the bed is not an option, we do have a solution. We use intraoral digital scanners as opposed to traditional impression materials, thereby eliminating the danger of material running down the patient's throat and ensuring a safe and efficient procedure.
The conclusion
A personalised and patient-centered approach to dental treatment is the fabrication of dentures in the patient's residence by a domiciliary dentist. At the Clinic for Implant & Orthodontic Dentistry, we strive to make this journey as pleasant and rewarding as possible, particularly for patients confronting unique obstacles. We have the knowledge and skill to create dentures that restore your smile and improve your quality of life. If you would like to schedule an initial consultation, please contact us at 01903-821822. We anticipate serving you and ensuring that your dental requirements are met with the utmost care and expertise.
Top 5 Sources of Dental Implant Pain When "There's Nothing Wrong with the Implant"- By Dr Amir Mostofi, DDs Dip MSc
Experiencing pain after a dental implant, even when everything looks fine? Explore the top 5 reasons behind post-implant discomfort and find solutions to ensure a comfortable journey towards a perfect smile.
If you've recently had a dental implant and are experiencing pain even though everything seems normal, you're not alone. This article aims to explain the top 5 reasons behind dental implant pain when there's no apparent issue with the implant itself, in a way that's easy for patients to understand.
1. Violations of the Inferior Alveolar Canal (IAC):
The IAC is a canal that houses the inferior alveolar nerve (IAN), which plays a crucial role in sensation for your lower jaw. Sometimes, the IAN takes a unique path, forming what's called an "anterior loop." Trauma to this area during implant placement can lead to sensory disturbances, bleeding, and pain. Recent research suggests that getting closer to the IAC may not be as risky as previously thought, as long as the nerve isn't directly affected.
2. Violations of Branches in the Mandibular Canal:
Traditionally, we've considered the IAC as a single canal to be avoided during implant surgery. However, it's now known that smaller branches can exist alongside the main canal, creating a network. If these branches are accidentally disturbed during surgery, it can result in pain. These branches are often missed because they aren't widely recognized, but they can show up on X-rays or CT scans.
3. Inadequate Keratinized Tissue:
Keratinized tissue is the protective, tough tissue that surrounds your implant crown. Some studies suggest that not having enough of this tissue (usually at least 2 mm wide) can lead to pain, especially when you touch or use the implant, like when brushing or eating. Fortunately, this issue can often be resolved by adding more tissue through a soft-tissue graft.
4. Poor Bone-to-Implant Contact:
Even if an implant looks fine on X-rays and CT scans, it's possible that the bone around it isn't providing a secure foundation. This can happen when fibrous tissue forms around the implant instead of sturdy bone. This may not be visible in regular exams, but patients can still feel pain when using their implant, especially when it's fitted with a crown. A resonance frequency analysis machine can help diagnose this issue by measuring the strength of the implant-bone connection.
5. Predisposing Risk Factors:
Sometimes, pain after implant surgery can be linked to factors that exist within your medical or genetic makeup. Conditions like fibromyalgia, temporomandibular disorders, and depression/anxiety can make you more prone to experiencing pain. This type of unexplained pain often falls under the category of "peripheral painful traumatic trigeminal neuropathy" (PPTTN).
In summary, if you're feeling pain after a dental implant, even when everything looks fine, it's important to consider these factors before assuming it's psychosomatic. There are various reasons behind implant-related pain, and a thorough evaluation is essential to pinpoint the cause accurately. Your dental professional can help you identify and address the issue, ensuring your dental implant journey is as comfortable as possible.